Anatomy and Cause

Should one ever find themselves rubbing the outer (lateral) region of the knee, it may be worth taking a moment to read and ponder the following about iliotibial band syndrome (ITBS).
In runners, ITBS is a leading cause of lateral knee pain with accounting to approximately 12% of all running related injuries and the second leading cause of overall knee pain (9, 4). It is a non-traumatic overuse injury thought to be caused by repeated flexion and extension of the knee which can irritate the structures around the knee joint. The constant friction of the ITB repetitively shifting or sliding forward and backward over the lateral femoral epicondyle (figure 2) can also cause inflammation of the ITB (10, 7).
Other causes may include extrinsic factors such as an increase in training volume, inappropriate shoe wear and lifestyle. Intrinsic factors such as an individual's flexibility, strength and running mechanics can also contribute (9). These factors will be viewed in more detail below.
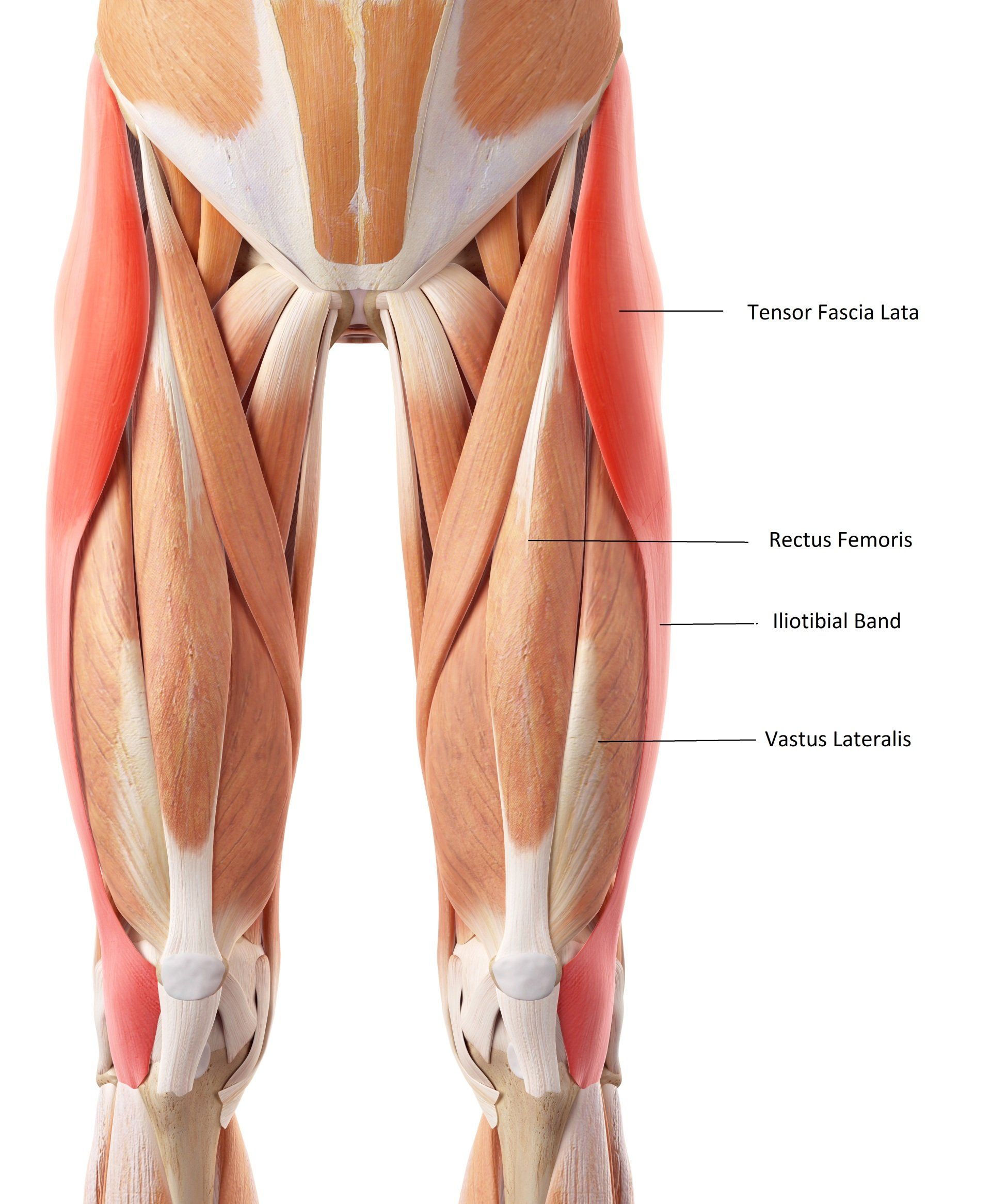
Figure 1
The Iliotibial Band and Anatomy
The ITB has been described as a “sheet of connective tissue” or large thick band of deep fascia and is a distal continuation of the fascia arising from the tensor fascia lata (TFL), gluteus maximus and gluteus medius muscles (figure 1) (1).
The dense connective tissue of the ITB assists stance stability and resists large varus torques at the knee, which may explain why this region becomes so tight in individuals with a varus tibiofemoral (bow-leg) strain (2). Iliotibial band syndrome occasionally becomes inflamed at its proximal origin and can cause referred hip pain.
The muscle is linked to the femur via strands of dense, regular fibrous connective tissue (3). After it courses between the biceps femoris and vastus lateralis, the ITB attaches to the lateral femoral condyle and sends lateral retinacular fibers to the patella (11).
The iliotibial band has two significant attachments including the lateral epicondyle, Gerdy's tubercle (at the anterolateral tibia) and the fibular head (figure 2).
The first iliotibial band attachment is into the distal edge of the femur at the upper edge of the lateral epicondyle which has a layer of adipose tissue underneath(2). The adipose tissue contains pacinian corpuscles which is highly vascular and may be the site of inflammation that causes pain during compression (2). Interestingly, certain movements can 'tug' at the Gerdy's tubercle attachment site when the muscle is tensed, especially during tibia internal rotation as the knee flexes during the weight-acceptance phase of gait (2).
The ITB has various other distal attachments which include the biceps femoris, vastus lateralis, lateral patellar retinaculum, patella and patella tendon (2). Collectively, these anterior and lateral attachments form a 'horseshoe pattern' or 'U shape' to provide anterolateral support to the knee (2). The site of injury is often associated with the insertion at the lateral epicondyle but interrelated with the forces created by the various attachments above and below the lateral epicondyle (Figure 2).
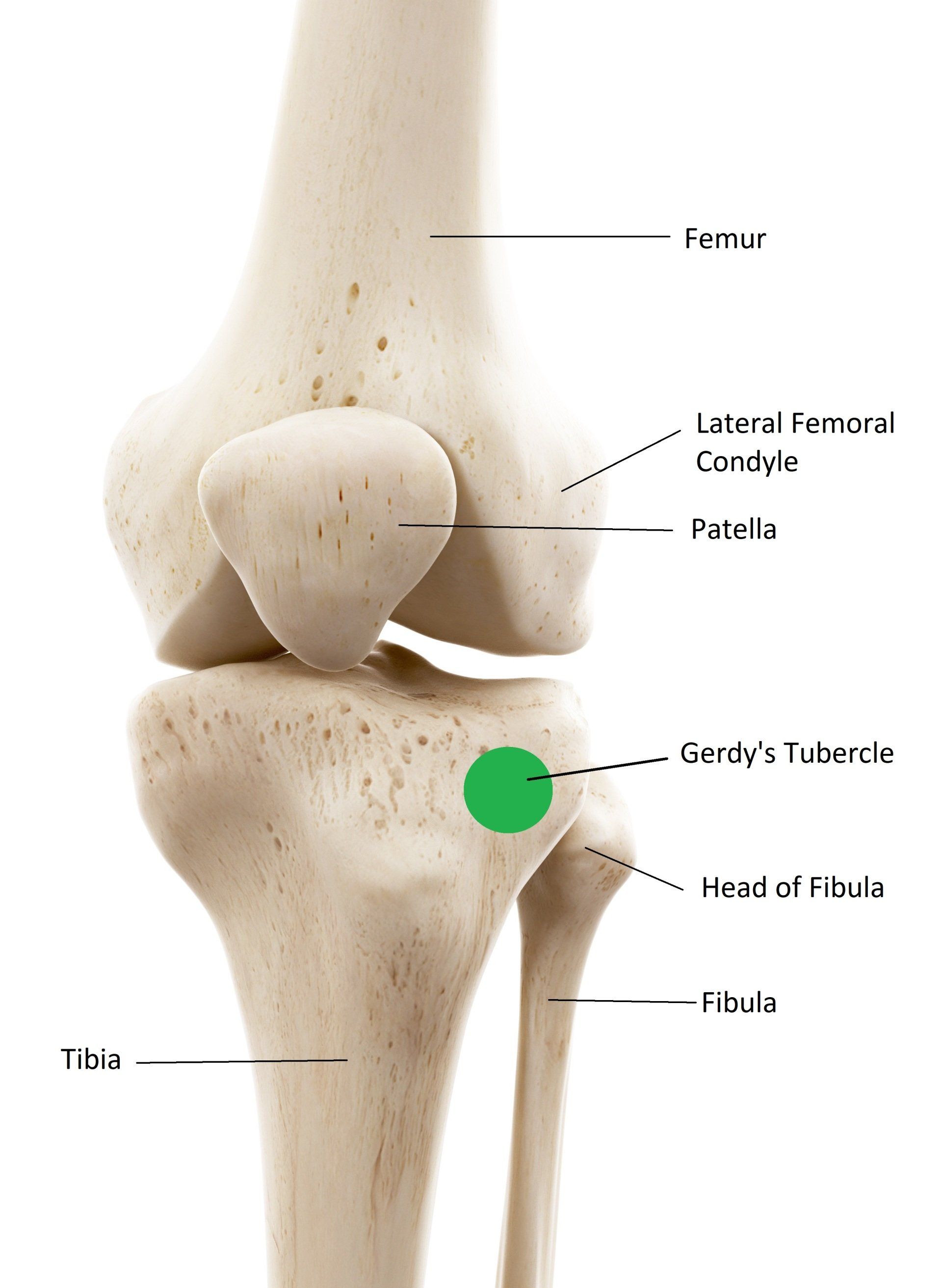
Figure 2
Intrinsic Contributing Factors To ITBS
Various intrinsic factors can attribute to ITBS and the following are signs that your therapist will be looking out for during a physical examination:
- Femoral external rotation during stance and gait cycle.
- Excessive hip adduction.
- Knee internal rotation.
- Leg length descrepencies.
- Increased foot inversion.
- Reduced Hamstring strength.
- Increased knee flexion at heel strike.
- Reduced hip abductor muscle strength.
- Weak hip abductors which can lead to increased hip adduction during stance phase of gait (7).
- Knee varus or valgus (knock-knee)strain.
- Shortenend and strengthened tensor fascia lata (postural muscle) which clinically tends to create increased flexion at the hip during stance phase and tends to increase hip internal rotation.
- A shortened (or taut) and over strengthened TFL which can dominate the weaker gluteus medius posterior and gluteus maximus, thus result in a compensated postural pattern including a Trendelenburg sign and compensated Trendelenburg sign (2).
(i.) Normal single-limb stance with the ground reaction force vector passing medially to the knee joint and producing a varus torque at the knee joint (2).
(ii.) Excessive hip adduction during single limb stance and a Trendelenburg sign, causing the ground reaction force vector to pass more medially, causing an increased varus torque at the knee joint, elongated lateral hip musculature which inctrease the stress on the ITB (2).
(iii.) Valgus stress at the knee joint causing the ground reaction force vector lateral to the knee which tends to create a more valgus strain to the knee joint, increased hip adduction and compensated Trendelenburg sign (with that there is no assymetrical alignment of the pelvis) (2).
Extrinsic Contributing Factors
Training Factors
These include:
- Excessive running; greater than normal weekly mileage
- Downhill running as the reduced knee flexion at foot strike increases friction between the ITB and lateral epicondyle.
Abnormal Walking Biomechanics
Biomechanical studies of runners with ITBS show that in the running cycle, the posterior edge of the ITB can impinge against the lateral femoral epicondyle of the femur just after foot strike in the gait cycle (6). This can produce irritation and subsequent inflammatory reaction, especially in the region beneath the posterior fibers of the ITB which are felt to be tighter against the lateral femoral condyle than the anterior fibers.
The symptoms usually come on after a reproducible time or distance run and consist of a sharp pain or burning on the lateral aspect of the knee. Occasionally, there will be swelling and thickening of the tissue where the band moves over the lateral femoral condyle.
Assessment
The Ober Test
The Ober test is the most commonly used to assess tightness of the iliotibial band which is performed via:
The examiner stands behind a side lying patient and stabilises the pelvis with one hand. The superior thigh is then moved into maximal abduction which is maintained in this position whilst moving the thigh into extension. The examiner lowers the limb into adduction until end range, or until the pelvis starts to tilt. The angle of hip joint adduction is considered to be a measurement of ITB length (7).
Angle of Knee Flexion During Stance Phase
Knee flexion at about 20-30 degrees is the usual knee range of motion at which the ITB is most likely to 'rub' against or compress underlying structures within the lateral femoral condylar region and create pain (7).
Treating ITBS
Stretch Application of the Tensor Fascia Lata
Wilhelm et al., (2017) studied the iliotibial band tensor fascia lata complex (ITBTFLC) elongation response to a simulated clinical stretch (in-vitro) and whether a “stretch” to the region translates into a clinically meaningful tissue elongation. The study found that greater lengthening occurred in the proximal region of the ITBTFLC, suggesting that the proximal region (containing the TFL) is more likely to undergo elongation in response to a clinical stretch force when compared to the middle or distal regions (11).
However, the increased lengthening response in the proximal region may be due to the presence of the TFL, suggesting that the ITB is incapable to elongate when applying passive stretching (11).
Massage Application of the ITB - Considered Ineffective
A study by Chaudhry et al., (2008) found that very large forces, outside the normal physiologic range of manual therapy, are required to produce even 1% compression and 1% shear in the tensor fascia lata (with9075N or 925 kg)and plantar fascia (4515N, 460 kg).Thus, further indicating that it is virtually impossible to physically elongate the length of the tensor fascia or ITB (3). For this reason, I have learnt that it is more effective to apply massage and physical therapy to the quadratus lateralis and gluteal muscles which are often tight.
Correcting Intrinsic Factors
Manual therapy might consist of correcting contributing intrinsic factors listed above. Strengthening exercises to address weakness within gluteus medius and excessive hip adduction and knee internal rotation or excessive knee varus or valgus strain.

More information and exercises can be read in the attached here.
References
1.) AiKhaund, R., Flynn, S. H. (2005) Iliotibial Band Syndrome: A Common Source of Knee Pain, 71; 9: 1545-1550.
2.) Baker, R. L., Souza, R. B., Fredericson, M. (2011) Iliotibial Band Syndrome: Soft Tissue and Biomechanical Factors in Evaluation and Treatment, Clinical Review: Current Concepts, the American Academy of Physical Medicine and Rehabilitation; 3: 550-561.
3.) Chaudhry, H., Schleip, R., Ji, Z., B, B., M, M., F, T. (2008)Three-Dimensional Mathematical Model for Deformation of Human Fasciae in Manual Therapy,JAOA; 108: 8.
4.)Fredericson, M., Cookingham, C. L., Chaudhari, A. M., Dowdell, B. C., Oestreicher, N., Shirley A. Sahrmann, S. A. (2000)Hip Abductor Weakness in Distance Runners with Iliotibial
Band Syndrome, ClinJ Sport Med; 3 (10): 169-175.
5.) Fredericson M., Guillet M., DeBenedictis L. (2000) Quick solutions for Movement Patterns. Iliotibial Band Syndrome. Phys Sportsmed, 28, 52-68.
6.) Fredericson, M., Wolf, C. (2005) Iliotibial Band Syndrome in Runners: Innovations in Treatment, Injury Clinic, Sports Med; 35 (5): 451-459.
7.) Lavine, R. (2010) Iliotibial Band Friction Syndrome, Humana Press; 3: 18-22.
8.) Miller, R. H., Lowry, J. L., Meardon, S. A., Gillette, J. C. (2007) Lower extremity Mechanics of Iliotibial Band Syndrome During An Exhaustive Run, Science Direct, Gait and Posture; 26: 407-413.
11.) Wilhelm , M., Matthijs , O., Browne , K., S eeber , G., Matthijs , A., Sizer , P.S., Brismée , J. M., James , R., Gilbert , K. K. (2017) Deformation Response of the ITB -Tensor Fascia Lata Complex To Clinic- Grade Longitudinal Tension Loading In-Vitro, Int J Sports Phys Ther.,12(1): 16–24.



