Osteoporosis
- by Joanna Blair
- •
- 08 Jun, 2025
- •
A Silent Threat To Bone Health

Osteoporosis is a chronic skeletal disorder characterized by a decrease in bone mass and deterioration in bone tissue, leading to increased bone fragility and risk to fractures. Often called the “silent disease,” osteoporosis progresses without obvious symptoms until a fracture occurs; commonly in the hip, spine, or wrist. As populations age globally, osteoporosis presents a growing public health concern, especially among postmenopausal women and the elderly.
Causes & Risk
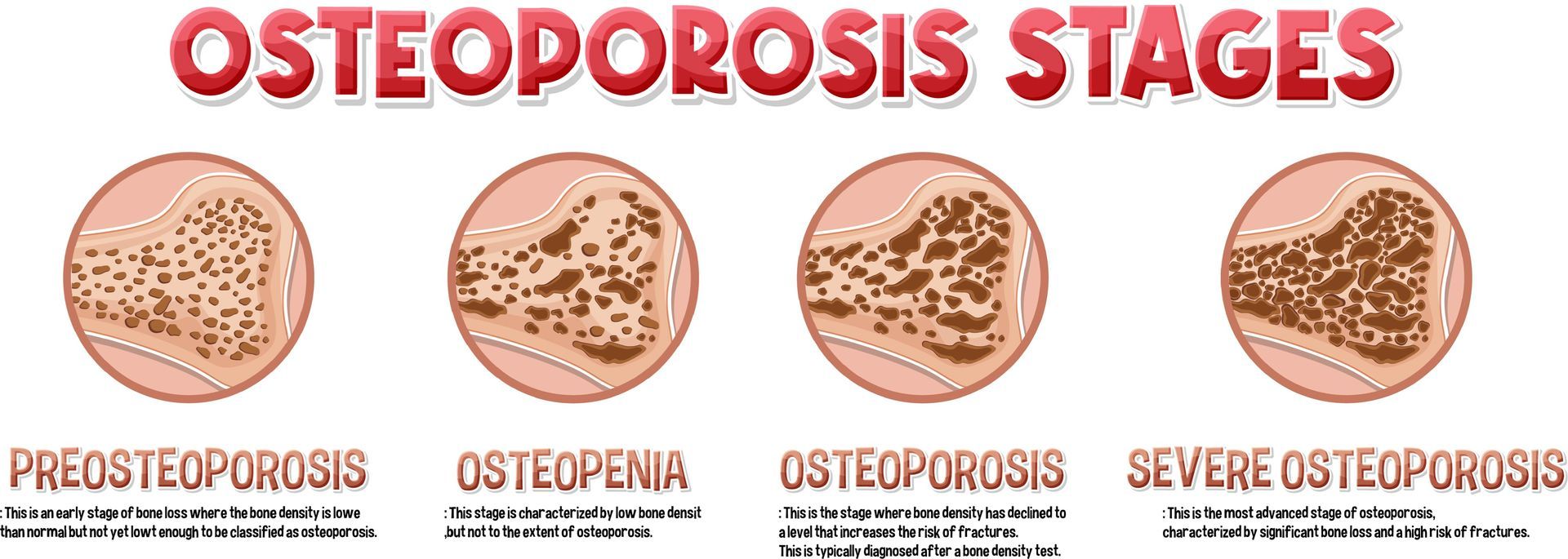
The development of osteoporosis involves a complex interplay between genetic, hormonal, nutritional, and lifestyle factors. Bones are dynamic tissues that continuously undergo remodeling, a balance between bone resorption (breakdown) by osteoclasts and bone formation by osteoblasts. In osteoporosis, this balance tips toward greater resorption, leading to porous, brittle bones.
The primary cause of osteoporosis in women is the drop in estrogen levels after menopause, which accelerates bone loss. In men, a gradual decline in testosterone can contribute. Other risk factors include inadequate calcium and vitamin D intake, sedentary lifestyle, smoking, excessive alcohol consumption, and a family history of osteoporosis. Certain medical conditions such as rheumatoid arthritis, and the use of corticosteroids, can also increase risk.
The societal burden of osteoporosis is significant. Fractures related to osteoporosis are a major cause of morbidity and mortality, especially in older adults. Hip fractures in particular often lead to hospitalization, surgery, and long-term care needs. According to the International Osteoporosis Foundation, one in three women and one in five men over the age of 50 will experience osteoporotic fractures in their lifetime. The economic costs, both direct and indirect, are substantial and growing.
Stages of Osteoporosis:
Symptoms and Diagnosis
How Might Osteopathy & Sports Massage Help? Prevention and Treatment

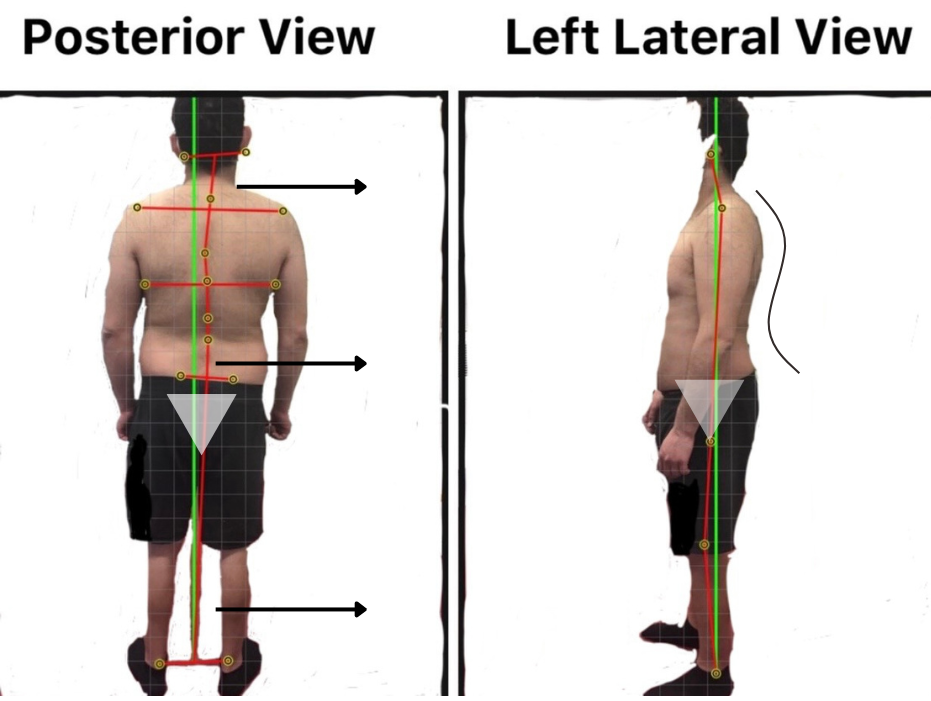
1. Postural Analysis / Postural and Alignment Improvements
Poor posture—especially kyphosis (rounded upper back)—can worsen the risk of vertebral fractures in people with osteoporosis. Osteopathy and postural analysis can help teach:
- An awareness of postural defects.
- Postural correction exercises
- Core strengthening routines
- Safe ways to sit, stand, and move without putting excess pressure on fragile bones
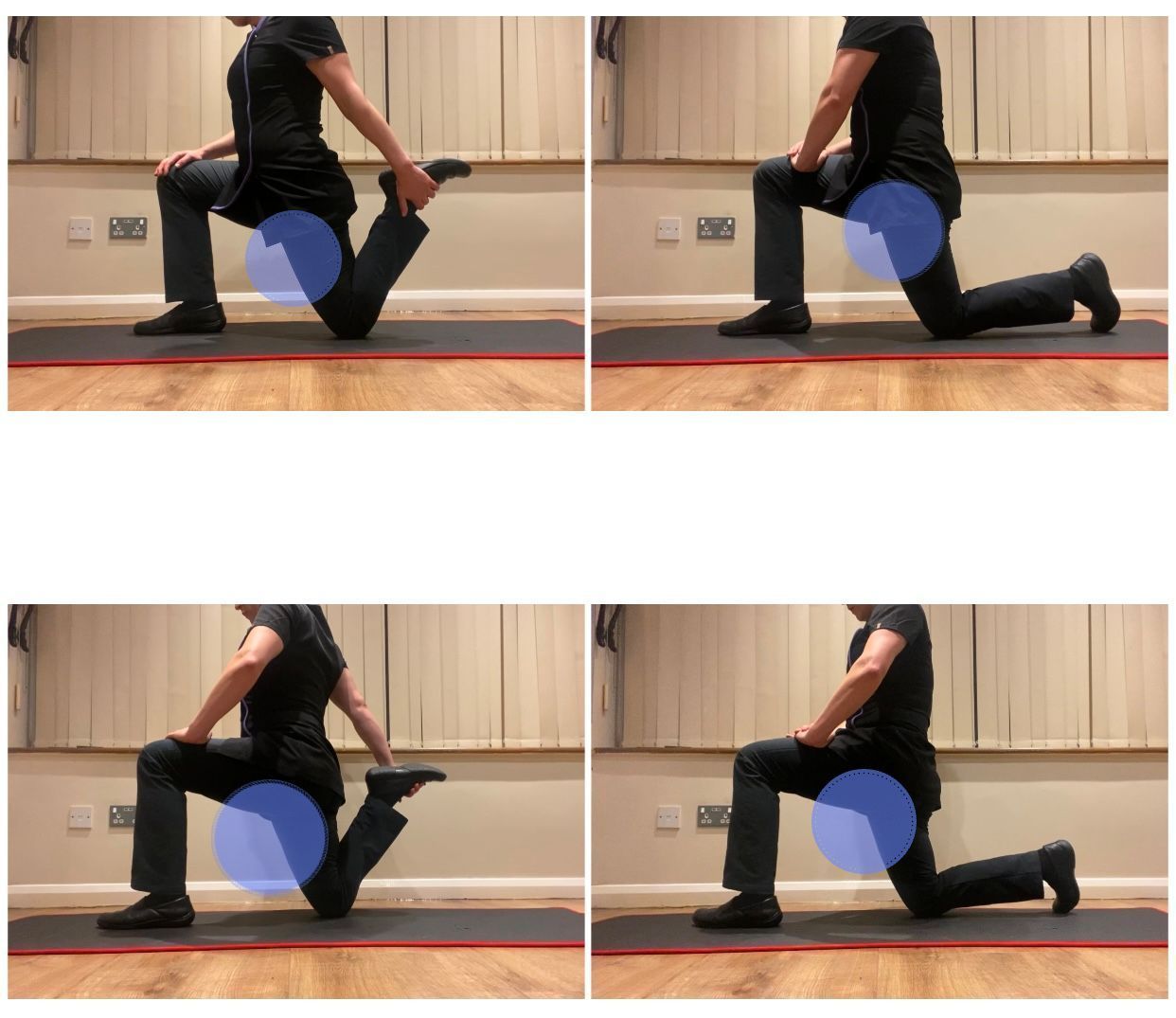
2. Increases Bone Density Through Weight-Bearing Exercise
Physical therapists design weight-bearing and resistance exercises tailored to each patient’s condition. These activities stimulate bone remodeling by encouraging the body to build more bone mass. Examples include:
• Walking or stair climbing
• Light weightlifting or resistance band training
• Tai chi and yoga (with modifications)
While physical therapy can’t reverse osteoporosis, it can slow its progression and help maintain current bone density.
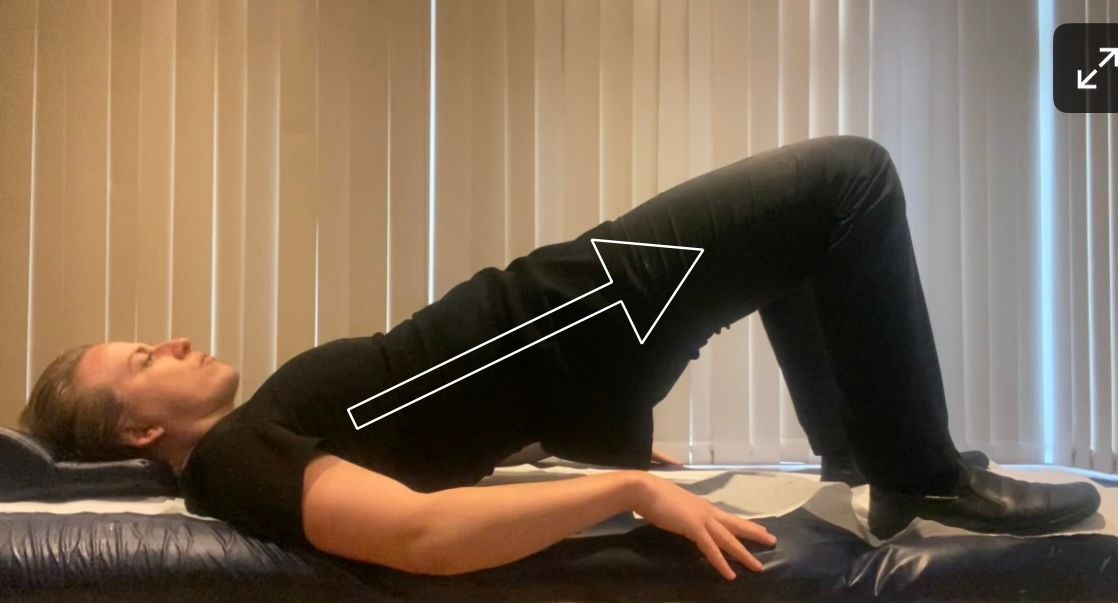
3. Enhances Balance and Prevents Falls
Falls are a leading cause of fractures in people with osteoporosis. Physical therapists assess balance and coordination, then design exercises to:
• Improve stability and lower limb strength
• Boost reaction time and proprioception (body awareness)
• Reduce fear of falling through confidence-building movement practice
4. Provides Safe Movement Education
People with osteoporosis may unknowingly move in ways that put them at risk. Physical therapists educate patients on:
• Safe ways to lift, bend, and carry
• How to avoid twisting motions that stress the spine
• Home safety modifications (e.g., removing trip hazards)
5. Reduces Pain and Improves Quality of Life
Chronic back pain from spinal fractures or muscle strain is common in advanced osteoporosis. Physical therapists use:
• Gentle stretching and mobility exercises
• Manual therapy techniques
• Pain management strategies (heat, cold, positioning)
6. Diet
Preventing osteoporosis involves addressing modifiable risk factors early in life. A diet rich in calcium and vitamin D, regular weight-bearing exercise, and avoiding smoking and alcohol can help build and maintain strong bones. For those at high risk or already diagnosed with osteoporosis, medical treatments may be necessary.
Pharmacological treatments include bisphosphonates, which slow bone resorption, and newer options like denosumab, selective estrogen receptor modulators (SERMs) and parathyroid hormone analogs that promote bone formation. Hormone replacement therapy (HRT) may be considered for some postmenopausal women, although it comes with potential risks.