Notes Made from The Following Studies;
Regularly asked questions in practise are "what are (muscle) knots?"
and " what causes them
?".
Revising and digesting the two studies above on their pathology and physiology will hopefully answer those questions and give a good scientific knowledge as to why they occur.
Muscle "knots" are clinically known as myofascial trigger points (MTrP)
and there is great confusion over what they are and the terminology, theories, concepts, and diagnostic criteria are
inconsistent, incomplete, or controversial.
What is Myofascial Pain Syndrome (MPS)?
- Shah et al., (2015) discusses myofascial pain syndrome (MPS) which is a fancy term used to describe painful muscle or surrounding connective tissue which can be acute (lasting less than 6 weeks) or chronic (lasting more than 3 to 6 months).
- MPS is an extremely common, but often overlooked source of muscle pain, discomfort, and dysfunction (Hoyle, 2006).
- Myofascial pain is characterized by contraction "knots" or "nodes" in the muscle that are hypersensitive on palpation, may stimulate local and/or referred pain, may elicit a local twitch response and may be eliminated by a local anesthetic or manual therapy.
- It is a complex disorder related to the development of myofascial trigger points in muscle. These myofascial TrPs have been further defined by their clinical characteristics as being either "active" or "latent".
- An "active" trigger point is associated with a clinical pain complaint.
- A "latent" trigger point is tender on palpation and may be associated with restricted range of motion and stiffness but is not associated with spontaneous complaints of pain (Hoyle, 2006).
What is fascia?
"Fascia is classified by layer, as superficial fascia , deep fascia , and visceral or parietal fascia, or by its function and anatomical location."
What is Myofascia?
The term “myofascial” describes how both muscle and fascia contribute to symptoms.
What Is A Myofascial Trigger Point (MTrP)?
- MTrPs are fined as "hard, discrete, hyperirritable, palpable nodules in a taut band of skeletal muscle that may be spontaneously painful (i.e. active) or painful only on compression" (Shah et al., 2015).
- An active MTrP is clinically associated with spontaneous pain in the immediate surrounding tissue and/or to distant sites in specific referred pain patterns.
- Strong digital pressure on the active MTrP exacerbates the patient's spontaneous pain complaint and mimics the patient's familiar pain experience.
- MTrPs can also be classified as latent, i.e. lay "dormant" or "hidden" and asymptomatic as the MTrP is physically present but has not created a spontaneous pain complaint.
- However, pressure on the latent MTrP elicits local pain at the site of the nodule.
- Latent and active MTrPs can be associated with muscle dysfunction, weakness, and limited joint range of movement.
History of MPS as a Diagnosis
- Guillaume de Baillous (1538-1616) of France was one of the first to write in detail about muscle pain disorders.
- In 1816, the British physician Balfour associated “thickenings” and “nodular tumors” in muscle with local and regional muscle pain.
- Froriep in 1843 coined the term “muskelshwiele” (muscle callouses) to describe what he believed was a “callus” of deposited connective tissue in patients with rheumatic disorders.
- In 1904, Gowers suggested that inflammation of fibrous tissue (i.e., “fibrositis”), created the hard nodules.
- Schade (1919) later proposed that the nodules, which he called “myogeloses”, were high viscosity muscle colloids.
- In the mid 1900s, important work was conducted independently by Michael Gutstein in Germany, Michael Kelly in Australia, and J.H. Kellgren in Britain. By injecting hypertonic saline into various anatomical structures such as fascia, tendon, and muscle in healthy volunteers, Kellgren was able to chart zones of referred pain in neighbouring and distant tissue.
- U.S. physician Janet Travell, whose work on myofascial pain, dysfunction, and trigger points is arguably the most comprehensive to date.
- Travell and Rinzler coined the term “myofascial trigger point” in the 1950s, reflecting their finding that the nodules can be present and refer pain to both muscle and overlying fascia.
- The current use of the term “MPS” implies a specific condition which presents as regional pain, sometimes with referred pain, often accompanied by increased tension and decreased flexibility.
- MPS has also been associated with other pain conditions including radiculopathies, joint dysfunction, disk pathology, tendonitis, craniomandibular (jaw) dysfunction, migraines, tension type headaches, carpal tunnel syndrome, computer-related disorders, whiplash-associated disorders, spinal dysfunction, pelvic pain and other urologic syndromes, post-herpetic neuralgia, and complex regional pain syndrome.
MPS Is Different To Fibromyalgia
- It is known to coincide with other diseases and syndromes associated with pain, e.g. rheumatic diseases and fibromyalgia.
- Unlike MPS, fibromyalgia is a widespread and symmetrically-distributed pain condition associated with sleep and mood disturbances.
- The pain of MPS is usually local or regional and may be found in a limited number of select quadrants of the body.
- MPS has traditionally been thought to present independently of mood or sleep abnormalities, recent studies indicate that MPS is associated with both mood and sleep disruptions.
- The definition and pathogenesis of MPS is still not fully understood, and disagreement persists as to whether MPS is a disease or process, rather than a syndrome.
Diagnosis For MTrPs; Not Straight Forward
- The current gold standard for the diagnosis of MPS is the physical examination as described in The Trigger Point Manual :
- Palpation of a taut band; Diagnosis of MPS has been tissue specific and anatomically based on palpation of the skeletal muscle for MTrPs.
- Identification of an exquisitely tender nodule (MTrP) in the taut band.
- Reproduction of the patient's symptomatic pain with sustained pressure.
- An MTrP is a common physical finding and often overlooked of non-articular musculoskeletal pain as its pathophysiology (explanation) is not fully understood.
- Digital palpation has several limitations. For instance, it lacks adequate sensitivity and specificity.
- Besides the use of palpation, there are currently no accepted criteria for identifying or describing MTrPs.
- Further research is needed to determine not only the role of the MTrP, but also its surrounding area.
- Diagnostic criteria are imprecise, and the full impact of MPS on life activity and function is not fully understood.
- To complicate this issue further, MTrPs are associated clinically with a variety of medical conditions including those of metabolic, visceral, endocrine, infectious, and psychological origin and are present across a wide range of musculoskeletal disorders.
- If the MTrP is frequently associated with other musculoskeletal pain syndromes, it would make this finding non-specific — if it is not, it would make the MTrP specific for MPS.
- Muscle pain displays unique clinical characteristics compared to cutaneous (skin) and neuropathic pain, the nature of the symptoms are highly dependent upon the individual's perception of its characteristic qualities (e.g., boring, aching, sharp, etc.), intensity, distribution, and duration.
- Characteristics like the quality of the pain, its distribution, and whether it radiates, have never been required for the diagnosis of MPS.
- Accurate diagnosis depends upon the examiner's clinical acumen, experience, index of suspicion, training, and palpation skills.
The Role of Muscle and The Cinderella Hyposthesis
- The Cinderella Fiber Hypothesis was first proposed by Hagg (1990) which explains how low level muscle damage could be brought on via low-threshold motor units (MUs) within muscles which are continuously activated during low level static exertions(LLSEs).
- Types of LLSEs or exertions are typically utilized by occupational groups such as office workers, musicians, hair dressers and dentists.
- "Cinderella" fibers are small low threshold muscle fibres which can become continuously overloaded and more prone to develop into myofascial trigger points since they are activated longer and are more likely to be metabolically exhausted before other fibres.
- A study by Treaster et al. (2006) supports the Cinderella Hypothesis by demonstrating that low-level, continuous muscle contractions in office workers during 30 minutes of typing induced formation of MTrPs.
- In contrast, larger motor muscle fibers do not work as hard and spend less time being activated.
- The "Cinderella" fiber theory, alone, fails to explain all aspects of injury related to LLSEs.
- It fails to explain the exact origin and mechanism of muscle pain as evidence suggests that muscle fiber activity and motor unit recruitment may be a consequence of pain rather than a cause.
- Low-threshold muscle fibers may fatigue and become metabolically exhausted but this does not explain how pain occurs.
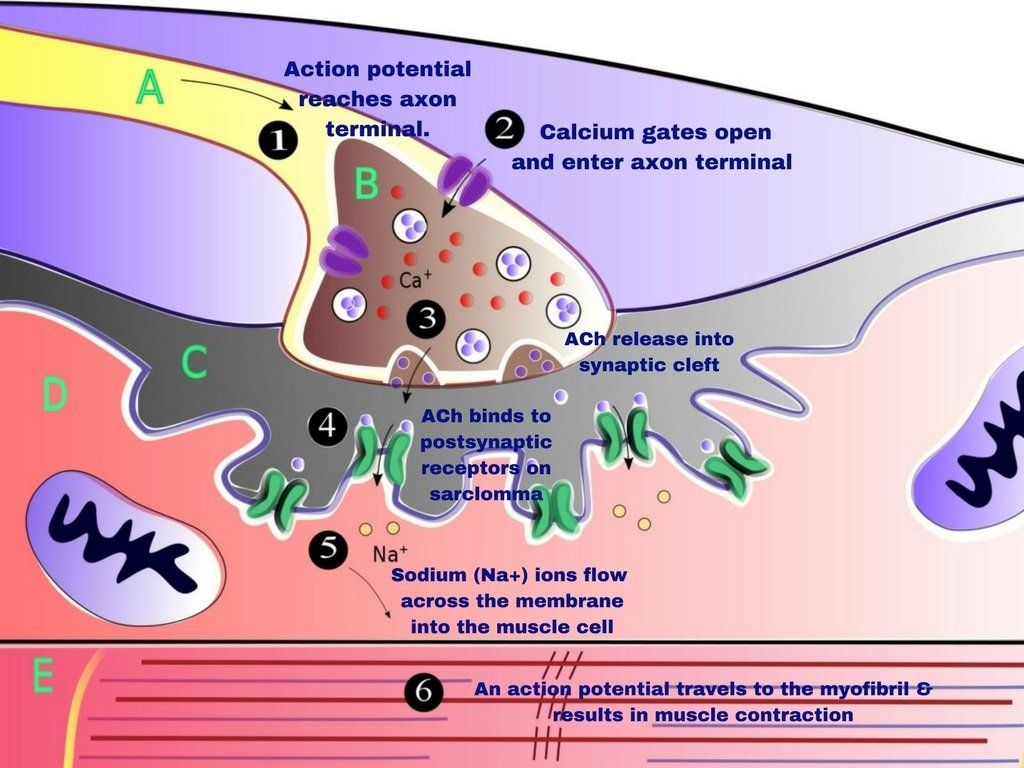
- A more widely
accepted hypothesis is that trigger points develop because some initiating event
causes an excessive release of acetylocholine (ACh) from the motor endplates resulting
in increased fiber tension and localized ischemia.
- The localized ischemia restricts the blood flow and insufficient ATP synthesis which is needed to restore energy.The increased demand and reduced supply of ATP forms the energy crisis and encourages the release of neuroreactive substances and metabolic byproducts (i.e., bradykinin (BK), substance P (SP), serotonin (5-HT)) which causes the peripheral nociceptors to become sensitive.
- Without ATP, the sarcoplasmic reticulum does not function correctly and the muscle sarcomeres remain contracted as the lack of energy (ATP) means that the the actin and myosin cross-bridges cannot disengage or release.
- ATP is also needed by the calcium (Ca2+) pump to remove calcium (Ca2+) from the muscle binding sites and restore them to the sarcoplasmic reticulum. Calcium (Ca2+) is needed and binds to troponin on the muscle fibers, which makes the muscle fibers contract.
- Localized areas containing "contraction knots" are believed to release sensitizing agents and additional acetylcholine (ACh) that cycles back to cause increased fiber tension.
- A feedback loop to maintain contraction is created and a self perpetuating cycle is established.
- Until this positive-feedback loop is interrupted, the muscle sarcomeres at the TrP remain in a shortened state, resulting in a local energy crisis.
Critique to the Energy Deficit Theory
- There is no explanation or description for the initiating event that causes the excessive release of ACh to occur in the first place.
- This theory also assumes that the motor endplates are the focus of attention for trigger point development.
- There is no evidence suggesting that the endplates are responsible for trigger point development.
- This theory fails to explain why MTrPs are more prevalent at certain 15 muscle locations than others.
Muscle Overuse and What Happens When Hyaluronic Acid (HA) Levels Rise
- HA functions as a lubricant that helps muscle fibers glide between each other without friction.
- With muscle overuse or traumatic injury, the sliding layers start to produce immense amounts of HA which then aggregate into supermolecular structures changing both its configuration, viscoelasticity and viscosity.
- Due to its increased viscosity, HA can no longer function as an effective lubricant which increases resistance in the sliding layers and leads to densification of fascia or abnormal sliding in muscle fibers.
- Interference with sliding can impact range of motion and cause difficulty with movement, including quality of movement and stiffness. In addition, under abnormal conditions, the friction results in increased neural hyperstimulation (irritation), which then hypersensitizes mechanoreceptors and nociceptors embedded within the fascia.
- This hypersensitization correlates with a patient's experience of pain, allodynia, paresthesia, abnormal proprioception, and altered movement.
References
Marieb, Elaine Nicpon; Hoehn, Katja (2007). Human anatomy & physiology
. Pearson Education. p. 133. ISBN
978-0-321-37294-9.
Shah, J.P., Thaker, N., Heimur, J., et al. (2015) Myofascial Trigger Points Then & Now: A Historical and Scientific Perpective. Physical Medicine and Rehabilitation,
7:746-61.
Treaster, D., Marras, W. S., Burr, D., Sheedy, J. E., Hart, D. (2006) Myofascial Trigger Point Development From Visual and Postural Stressors During Computer Work.
J Electromyogr Kinesiol. Apr;16 (2)
:115–124.



