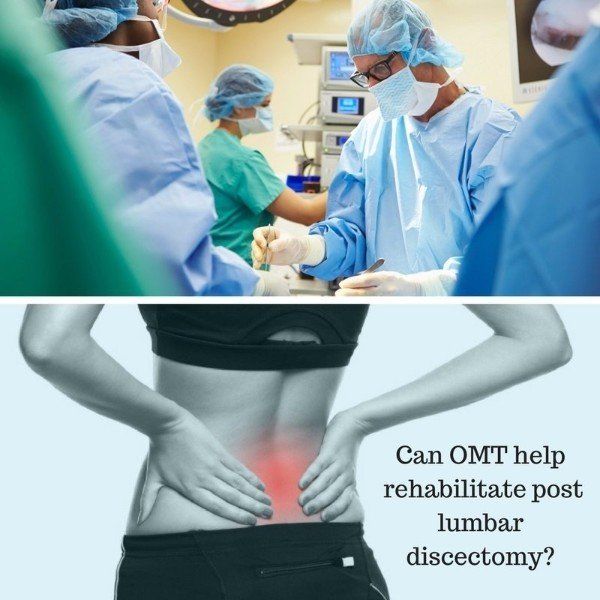
Rehabilitation with Osteopathic Manipulative Treatment (OMT) after Lumbar Disc Surgery randomised, Controlled Pilot Study, Summary and Short Critique
- by Joanna Blair
- •
- 06 Jul, 2017
- •
ByunghHo J. K., JungHoon, A., HeeCheol, C.,
DongYun, K., TaeYeong, Kim., BumChul, Y. (2015)
Rehabilitation with Osteopathic Manipulative Treatment (OMT) After Lumbar Disc Surgery: A Randomised, Controlled Pilot Study, IJOM: 18;
181-188.
Study Summary:
- 33 patients who had underwent lumbar microdiscectomy were randomly assigned to one of two intervention groups; either exercise programme or an OMT group post surgery.
- Both intervention programmes (Exercise and OMT) consisted of 8 individual sessions which were performed twice a week for 4 weeks.
- Each session was 30 minutes and all patients in both groups were prescribed supplementary anti inflammatory medication, analgesics and a muscle relaxant by surgeon.
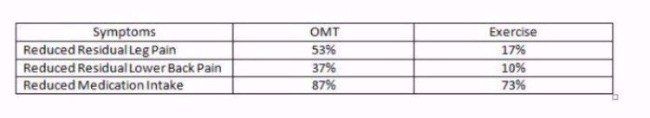
- Results showed reduced residual leg pain after the lumbar discectomy in the OMT group with a 53% reduction compared to the exercise group which had a 17% reduction.
- Residual lower
back pain
also decreased in both interventions with a 37% reduction in the
OMT group and a 10% reduction in the exercise group.
- No side effects or complications from any
intervention were reported.
- Patients in the groups required less frequent use of medication with an 87% reduction in the OMT and 73% in the exercise.
An overall improvement was found in the lumbar spine active ROM with patients being able to move without pain in both the OMT group and exercise groups.
Introduction
- Low back pain is a worldwide health problem with a lifetime prevalence rate of 80% and can affect daily physical activity (1.).
- Lumbar disc pain accounts for less than 5-10% of lower back pain (LBP) and is one of the most common reasons for lumbar spine surgery (2).
- Lumbar discectomy is one of the most commonly performed operations for lower back pain to relieve nerve root pain and reduce physical disability.
- The most common unsatisfactory complaints complications observed in patients following lumbar discectomy are;
- Continued post operative physical disability affecting daily activities.
- Residual lower back pain and leg pain (3.).
Post surgical intervention has been considered important to reduce post surgical physical complications and increase the success rate for patients post surgery.
This study performed a pilot study comparing Osteopathic Manipulative Treatment (OMT) with exercise following lumbar disc surgery to assess the feasibility for a future randomised control trial.
Study Method
- 48 patients who met the eligibility criteria and wanted to participate in the study were interviewed and screened by two research surgeons.
- The study was a randomised controlled pilot study and conducted at a major metropolitan spine surgery hospital where all participants underwent lumbar microdiscectomy.
- Two research spinal surgeons registered in Korea and a research osteopath registered in the UK conducted patient recruitment and screening.
- The study protocol was approved by the institutional review board of the University of Korea, and all participants provided written informed consent.
- Patients between 20 and 65 years of age who had lower back pain and referred leg pain resulting from a herniated lumbar disc and underwent lumbar microdiscectomy were identified by hospital nurses.
Patient Exclusion Criteria:
- A requirement of revision surgery or other forms of combined surgery.
- A refusal to participate
- Contraindication for participation including pregnancy, metastatic disease, or a mental disorder.
- Of the 48 patients, 15 were excluded and the remaining 33 were randomly allocated to either the OMT group or the exercise programme group.
Study Procedure
- 33 patients who had underwent lumbar microdiscectomy by 2 neurosurgeons at the spine surgery hospital returned to the hospital 2 to 3 weeks after surgery for baseline measurements and the first rehabilitation intervention.
- Each participant was randomly assigned to one of two intervention groups; either exercise programme or an OMT group.
- The allocations were conducted using simple randomisation.
- Both intervention programmes (Exercise and OMT) consisted of eight individual sessions which were performed twice a week for 4 weeks. Each session was 30 minutes and all patients in both groups were prescribed supplementary anti inflammatory medication, analgesics and a muscle relaxant by surgeons.
Intervention OMT Rehabilitation & Techniques Used:
- All patients underwent physical assessment before each intervention.
- The same practitioner applied a combination of techniques in the standardised protocol for the OMT but the intensity and sequence of the techniques were modified for each patient depending on their tolerance to treatment and other post-operative physical conditions.
- The protocol did not include spinal high-velocity, low-amplitude thrust (HVLAT) manipulation of the lumbar segments where the surgery was performed.
- The focus of the OMT protocol was to reduce biomechanical overload on the lumbar spine by functionally improving the motion of adjacent spinal segments or joints including the thoracic and cervical segments and the sacroiliac joint.
- The protocol included techniques applied to myofascial structures to reduce post-operative physical tension and stiffness generated in the body.
- Each OMT intervention was performed by two osteopathic students under the supervision of a qualified osteopath.
- Each treatment process was documented and reviewed by a research osteopath and surgeon.
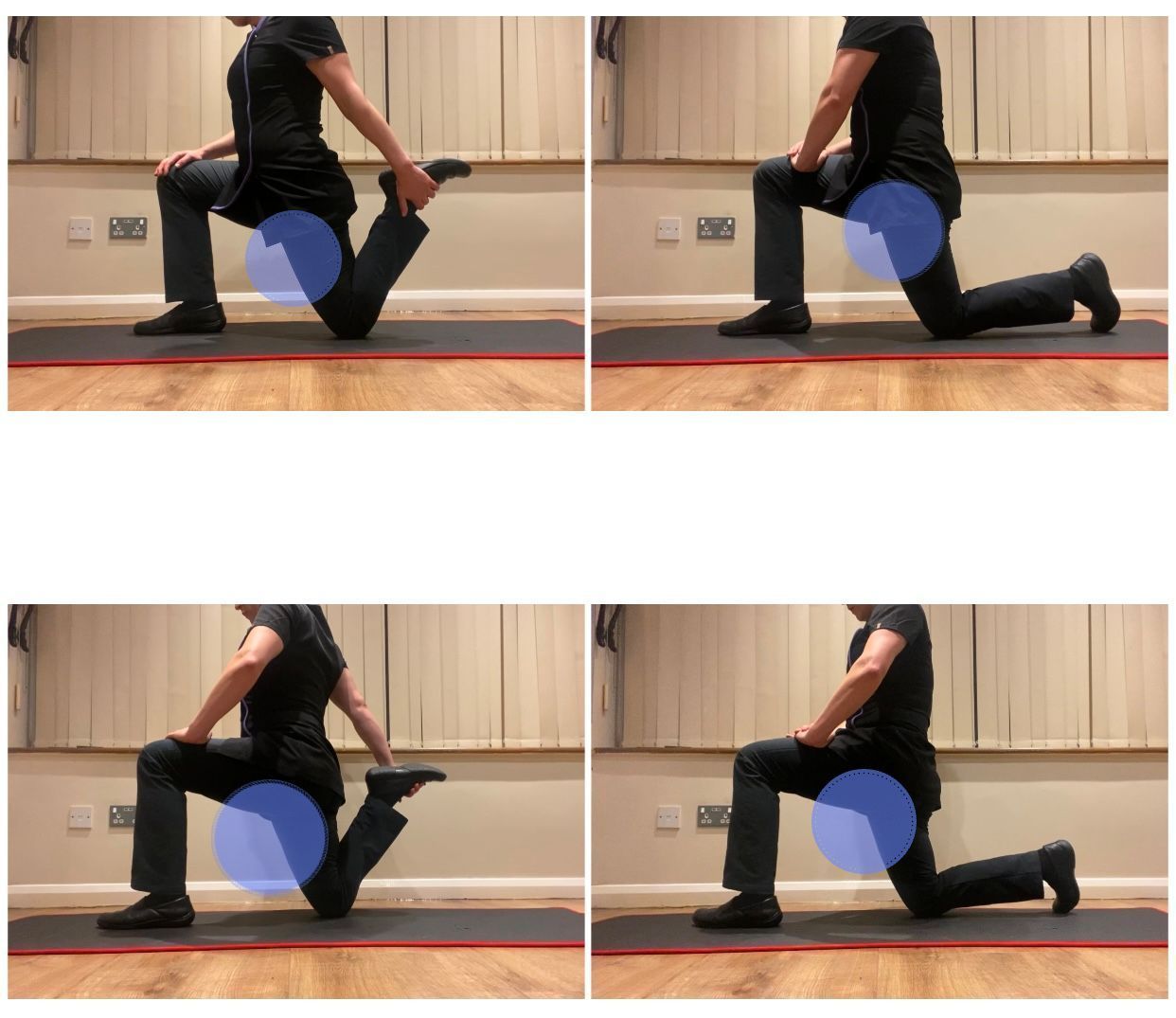
Exercise Programme
- Overall, 8 exercise sessions were conducted over a course of 4 weeks.
- The aim of the exercise programme was to improve spinal mobility and stabilise the lumbar segments.
- For the first week, practitioners focused on stretching exercises for the back and abdominal muscles with the patient in the supine position.
- For the 2nd and 3rd week, practitioners focused on isometric strengthening exercises for the back and hip extensors with the patient in the prone position or sitting on a gym ball.
- In the final 4th week, the intensity of the previous exercises was increased and back stability exercises were performed using a pilates exercise apparatus.
Outcome measures
- Outcome measures were assessed after 2 and 3 weeks post surgery and post-intervention.
- A post-intervention evaluation was conducted 7 to 8 weeks post surgery which was otherwise a week after the final rehabilitation session.
- Primary outcome measures were evaluated for post-operative disability and residual pain in the legs and lower back.
- Outcome measure questionnaires used were the Rolande Morris Disability Questionnaire (RMQ) with a 24-point scale and the Visual Analogue Scale (VAS) with 0 indicating ‘no pain’ and 100 indicating ‘the worst pain’.
- Secondary outcomes included lumbar range of motion (ROM), use of medication, and patient satisfaction.
- The lumbar spine ROM at which the patients could move without pain was measured with a double inclinometer by a physiotherapist who was not involved in any intervention.
- The number of supplemental medications taken per week was used to assess medication consumption.
- Patients were also asked to fill in a self-grading questionnaire to evaluate their satisfaction for their rehabilitation intervention which indicated ‘dissatisfaction’, ‘moderate satisfaction’ and ‘total satisfaction’.
- Patients were asked whether they would recommend the rehabilitation intervention they received to a family member or friend with a similar condition.
Statistical Analysis
- The Shapiroe Wilk test was used to assess normality of distribution of the data. Medians are shown for the range of movement found in lumbar spine extension and left side-bending, and for the number of times medication was used.
- The categorical data was analysed using the chi-square test or Fisher’s exact test to account for baseline variations.
- The Student‘s t-test or the Manne Whitney U test was applied to compare the differences between the groups. SPSS statistical software (Version 12.0, SPSS Inc., Chicago, IL) was used for the analyses. Two-sided tests and a significance level of 0.05 were used for all statistical analyses.
- Subjects Of the 48 patients deemed eligible for inclusion, 33 (69%) were enrolled and randomly allocated to either the OMT or exercise group.
- There were no significant differences in baseline characteristics and baseline measures between the two groups.
- The primary reason for non-enrolment was lack of interest in participation. Of the enrolled patients, 6% were lost to follow-up at the primary study endpoint (2 of 33, 1 in each group). All 33 patients who were randomly assigned to a group were analysed on an intention-to-treat basis.
Primary Outcome Results
- Primary outcomes OMT and the exercise programme improved all primary outcomes.
- Post-surgical physical disability questionnaire results showed that patients improved more after OMT rehabilitation than the exercise group.
- Residual leg pain after the lumbar discectomy decreased in the OMT group with a 53% reduction compared to the exercise group which had a 17% reduction.
- Residual lower back pain also decreased in both interventions with a 37% reduction in the OMT group and a 10% reduction in the exercise group.
Secondary Outcome Results
- An overall improvement was found in the lumbar spine active ROM with patients being able to move without pain in both the OMT group and exercise groups.
- Patients in the groups required less frequent use of medication with an 87% reduction in the OMT and 73% in the exercise.
- Patients in both groups responded that they were highly satisfied with the post-operative rehabilitation and answered that they would recommend the post-operative rehabilitation to a family member or a friend undergoing spinal surgery.
- No side effects or complications from any intervention were reported.
Table Of Results
Discussion
- In this pilot study, we showed the feasibility of OMT for post-operative rehabilitation after lumbar disc surgery compared to an exercise programme.
- The early post-operative physical disability and residual pain in the lower back and legs were reduced by both rehabilitation interventions.
- These two post-operative cares also improved the active range of motion of the lumbar spine and were shown to be a safe approach without side effects and high satisfaction.
- To the author’s knowledge, this is the first pragmatic, randomised, controlled pilot trial to assess the feasibility of OMT for post-operative rehabilitation after lumbar disc surgery.
- The present pilot study also showed the applicability of the combination of lumbar disc surgery and OMT rehabilitation in a pragmatic setting where the medical professionals including spinal surgeons, physiotherapists, nurses and an osteopath were involved in the study procedure.
Study Limitations & Critical Analysis
Summary Follow Up:
- It is difficult to determine whether the post-operative outcomes of OMT rehabilitation can be maintained long-termly because of a short follow-up duration.
- However, the information regarding the short-term beneficial effect of the early applied rehabilitation would be important because the main expectations of patients undergoing lumbar microdiscectomy are early return to work or normal daily activities after disc surgery.
Technique Use;
- Osteopathy is a patient-centred system of healthcare with individualised diagnosis and treatment. The manipulative techniques are only part of a philosophy of care.
- The unavailability of fully trained osteopath but osteopathic students to perform OMT intervention was also a study limitation.
- However, the intensity, sequence and selection of the treatment techniques were individualised to each patient depending on their physical conditions such as tolerance to treatment on the day of the intervention within the standardised OMT protocol.
- The research osteopath who was fully trained and registered and surgeon reviewed the each assessment for the treatment and supervised the OMT rehabilitation when required.
Lack of Blinding:
- The lack of blinding was also a methodological weakness. In the pragmatic study, however, it was not possible to prevent the patients from knowing the rehabilitation interventions.
- We explained the type of rehabilitation being used upon inquiry. In particular, the patients allocated to the OMT group were not familiar with osteopathic treatment.
Lack of Placebo
- Since the lack of a placebo control group, the
study result is limited to determine whether the post-operative outcomes were
improved by the interventions themselves or whether they were related to other
aspects of the interventions.
- Factors such as time spent with patients or frequency of patient’s visits may represent placebo effects.
- However, it was not desirable to use a sham treatment or no treatment because of ethical considerations concerning loss of chance for patients to improve the early post-operative outcomes.
- In addition, it is difficult to develop an OMT placebo at a pragmatic setting.
- The results presented in this pilot trial comparing OMT with exercise will be valuable because the exercise programme we applied in the study has proven to be more effective rehabilitation to improve early post-operative disability and pain than no treatment, or other types of interventions such as self-homecare or programmes focusing on behaviour treatment.
- Regarding timing and intensity of the rehabilitation, found that an intensive programme starting immediately after lumbar discectomy had better short-term outcomes such as pain reduction and increased range of lumbar motion than less active programme.
- This was further confirmed by experimental studies showing that vigorous exercise started 4 to 5 weeks postoperatively reduced physical disability and residual pain after lumbar disc surgery.
- Findings from the present study are limited but support the feasibility for a future definitive trial.
- The future well-designed, adequately powered trial will require a larger sample size and long term follow-up periods to confirm the effect of OMT rehabilitation.
- The use of fully trained and experienced osteopaths for the intervention should be considered in future research assessing the post-operative effect of OMT.
- The postoperative pain and its associated physical disability were more reduced in OMT, which required less use of medication; therefore a cost effectiveness analysis should be performed.
References:
1. Walker BF. The prevalence of low back pain: a systematic review of the literature from 1966 to 1998. J Spinal Disord Tech 2000;13:205e17.
2. Singh V, Manchikanti L, Calodney AK, Staats PS, Falco FJE, Caraway DL, et al. Percutaneous lumbar laser disc decompression: an update of current evidence. Pain Physician 2013;16:SE229e60.
3. Atlas SJ, Keller RB, Wu YA, Deyo RA, Singer DE. Long-term outcomes of surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: 10 year results from the Maine lumbar spine study. Spine 2005;30: 927e35.