Posture of The Head, Shoulders & Thoracic Spine In Comfortable Erect Standing; Summary and Short Critical Review.
- by Joanna Blair
- •
- 02 Aug, 2017
- •
Article written by Sally Raine and Lance Twomey (1994).
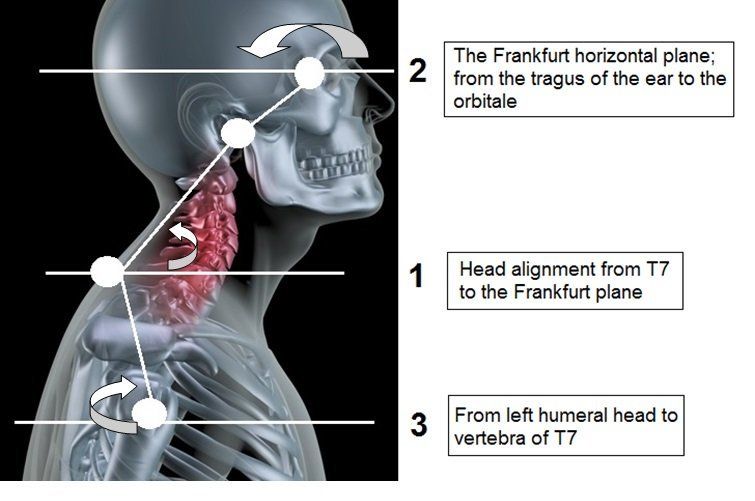
Figure 1
Short Study Summary:
- The following study explored the importance of posture in relation to dysfunction and pain in the cervical and thoracic spine.
- The reliability of postural measurements of the head, shoulders and thoracic spine were studied in 39 young healthy adults.
- Results overall showed that forward head posture and upper cervical spine extension tended to increase the kyphosis of the upper thoracic spine. Forward head position was not necessarily found to be related to a forward shoulder position nor upper cervical spine extension.
Method:
- 39 volunteers (31 female and 8 male) ranging in age from 17-48 years with an average of 22 years old participated in this study.
- 6 measurements of posture were obtained.
- Measurements of the subjects’ weight and sitting height (mm) were obtained.
Measurements:
1.) Anterior head alignment;
Points Measured:
- Inferior margins of the left and right ears.
- 180 degree angle meant a horizontal and aligned head.
2.)
Anterior Shoulder Alignment
Points Measured:
- Left and right coracoid process.
- A 180 degrees angle meant that the shoulders are held at the same level.
3.) Sagittal (lateral) Plane Head Alignment
Points measured:
- Between vertebra C7 to the tragus of the ear.
- When the angle of degrees value reduced, a more forward head position was described.
4.) Head Alignment from the Frankfurt Plane (Figure 1)
Points Measured:
- Between posterior margin of the tragus of the ear to the orbitale.
- An angle of 180 degrees represented the Frankfurt horizontal plane and described the head position to be horizontal.
- An angle less than 180 degrees meant that the orbitale was superior to thetragus and the upper cervicalspine was relatively extended.
- An angle greater than 180 degrees meant that the orbitale was inferior to thetragus of the ear and the upper cervical spine was relatively flexed.
5.) Sagittal Plane Shoulder Alignment
Points Measured:
- C7 vertebra and the humeral head of the left shoulder.
- The lesser the angle between two points meant the more rounded position of the shoulder.
6.) Upper and Lower Thoracic Curvature:
- Regions C7-T6 and T6-T12 (upper and lower regions of the thoracic spine)
- Heights if curves were measured during a sitting position.
7.) Weight and Sitting Height
Results;
- Each subject was measured in kgs.
- Two photographs were taken of each subject whilst standing and taken from the person's side on and frontal view (Figure 3 and Figure 4 in the study article).
- When the orbitale (eye socket) was held more superiorly with respect to the tragus of the ear, the shoulders were positioned more forward (held in protraction).
- A correlation was found between increased extended upper cervical spine and protractedly held shoulders.
- When the resting head position is anterior (forward head lag) with respect to C7, an increased curvature of the upper thoracic spine results.
- Supported the observation that people, overall tend to demonstrate asymmetrical shoulder height in the coronal (vertical) plane.
- Increased extension of the upper cervical spine meant a slight upward tilt of the orbitale from the Frankfurt horizontal plane (Figure 1).
- No significant difference was found between men and women for head and shoulder posture.
- No significant difference was found between men and women for the measurement of upper thoracic curvature.
- A difference was found between men and women for lower thoracic curvature.
- The average resting shoulder posture of subjects in the study was 47.6 degrees which represented a protracted resting position of sagittal (lateral) plane shoulder alignment.
- The position of the head in the sagittal plane was found to be related to the curvature of the upper thoracic spine. If the head was positioned more anteriorly with respect to the trunk, an increased flexed curvature between C7-T6 was found (increased thoracic spine kyphosis).
- A forward head posture did not indicate forward or protracted shoulders as may have been expected when measured with respect to the trunk. The results did not support the observation that a forward head is always associated with rounded shoulders.
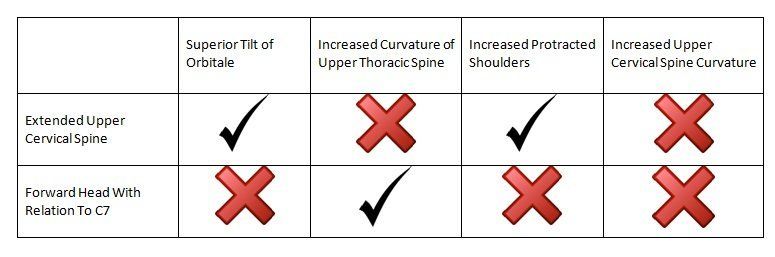
Short Table Summary of Study Findings;
Conclusion:
- Overall, a forward head posture and upper cervical spine extension tended to increase the kyphosis of the upper thoracic spine. However, the results for the correlative relationships was not found to be significant.
- A forward head position was not necessarily found to be related to a forward shoulder position nor upper cervical spine extension when measured in the sagittal plane.
Short critical analysis;
- This was a small scale study with 39 healthy, young volunteers involved.
- The majority of individuals were female (31 female and 8 male) with an average of 22 years of age.
- A larger study with a even number of males and females would have been required to possibly gain a more significant result.
- This article was published in 1994 and it would be interesting to study the difference with regards to technological advances since then for measuring posture.
Journal Reference: