Lower Back Pain & the Sacroiliac Joint
- by Joanna Blair
- •
- 29 Mar, 2019
- •
History, Anatomy & Cause
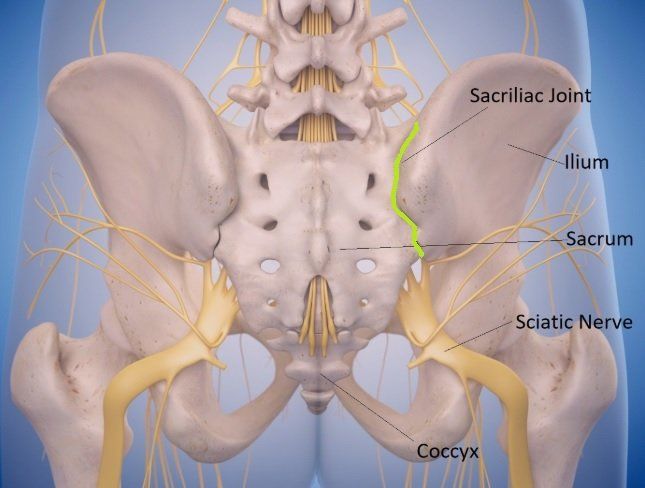
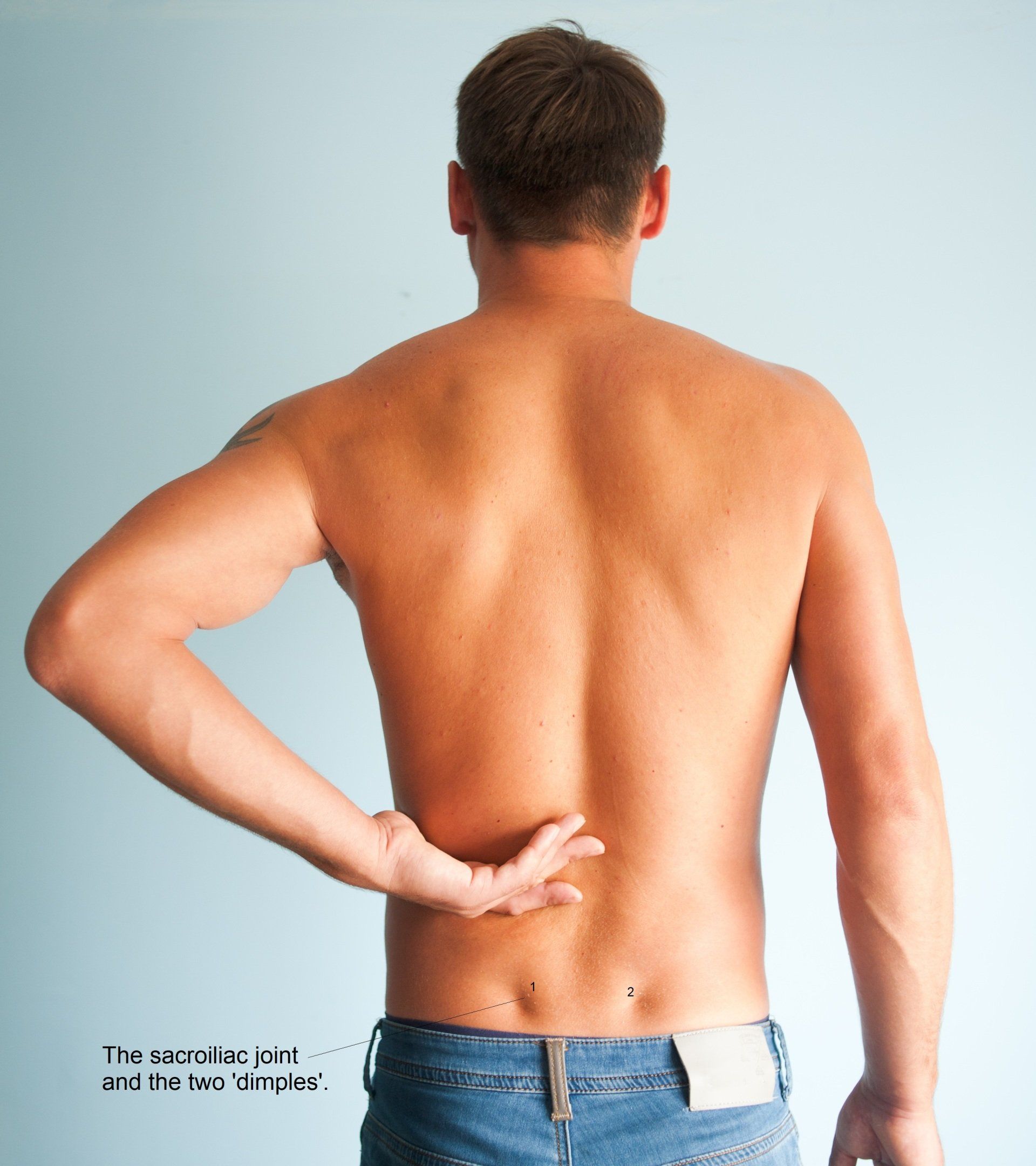
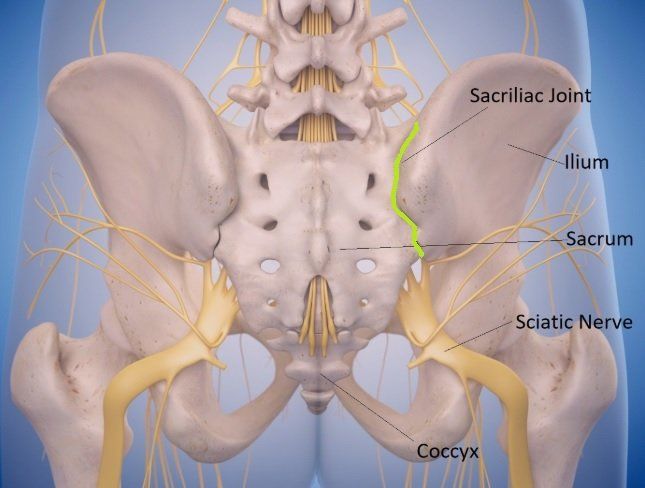
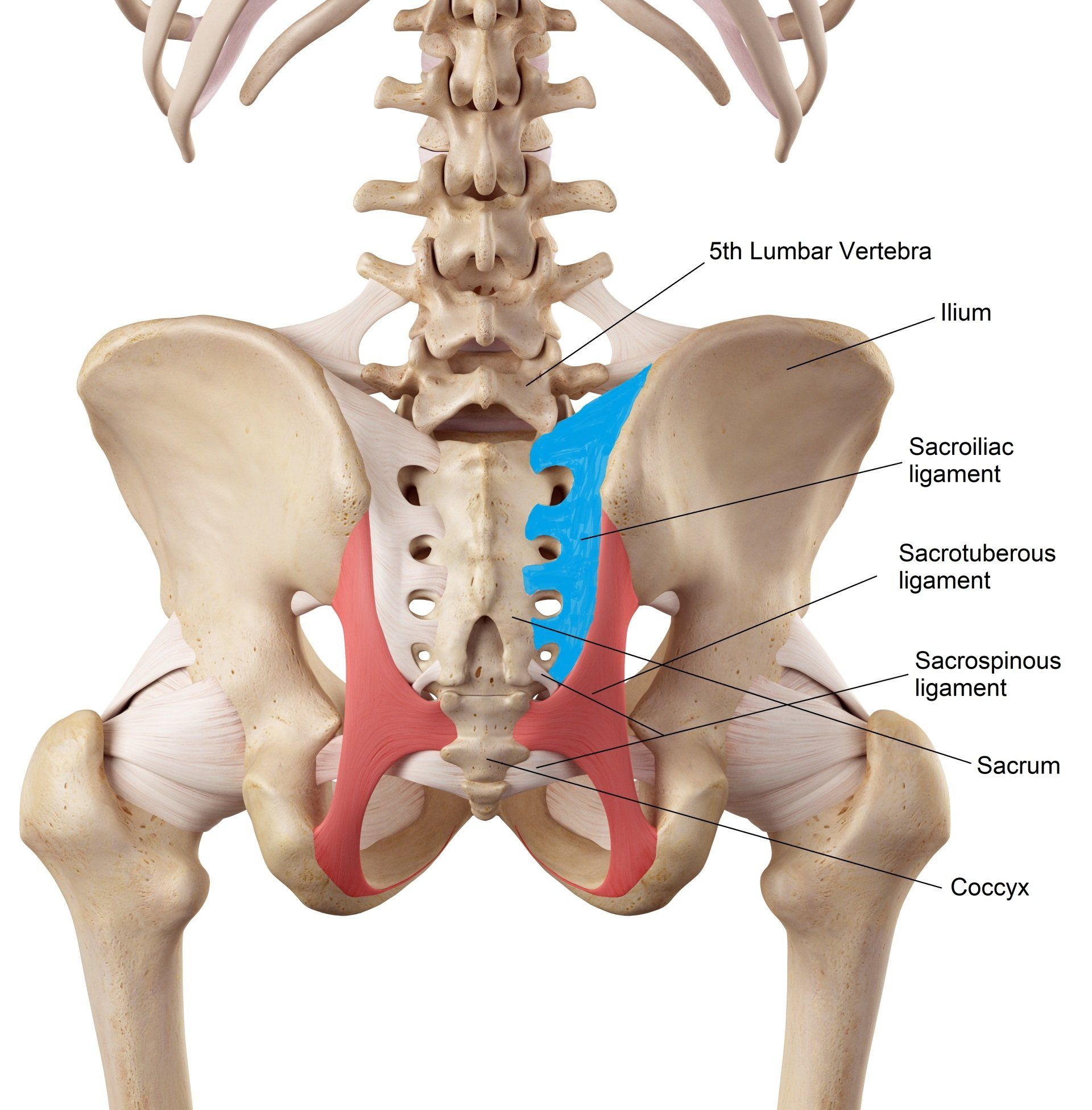
There are two sacroiliac joints in the body which are located between the iliac bones and the sacrum and connect the spine to the hips (figure 2). They provide a major role for support, stability and shock absorption during impact whilst walking and lifting.
Cohen et al., (2013) describe SIJ pain as an underappreciated but common cause of chronic lower back pain (LBP) and pelvic girdle pain (PGP) which can be presented in various different ways which is why making a diagnosis can be challenging. Understanding the condition's anatomy, clinical presentation and methods for assessment is important to make an accurate diagnosis, determine the source of pain and increase the likelihood of optimising a successful and faster recovery (2).
History of SIJ Pain
The sacroiliac joint was first described as a painful entity in 1905 and was found to be the primary source of lower back pain during the first third of the 1900s with little attention given to other biomechanical structures of the spine to cause pain in the lower back (7).
It was not until 1979 that fluoroscopic injection was considered as a form of pain prevention and therapeutic purposes to the sacroiliac joint(7).
Ageing & Development
Embryologically, the joint presents itself at the 10th week of gestation and is firmly established by the 16th week. The joint is well-defined anteriorly but posteriorly the joints are suspended by various ligaments (figures 4 and 5) (7).
In the first ten years of life, the SIJ enlarges its surfaces, remains flat and the anterior capsule thickens. After puberty, most individuals develop a ‘crescent shaped’ ridge along the length of the iliac surface which help lock the surfaces together to increase joint stability (12).
As we age, the joint surfaces become more irregular, rougher and prominent, possibly as an adaptation from adolescent weight gain, but the changes represent functional adaptations rather from a pathological cause (12).
The fibrocartilage covering the iliac side of the joint begins to consistently degenerate, usually by the third decade in males and the fourth or fifth decade in females. Narrowing of the joint space, cysts or osteophytic formation of the iliac side might be viewed on x-rays or CT scans, but the changes are usually asymptomatic. Interestingly, osteoarthritic changes are rarely evident on the sacral side by the fifth decade (12).
The connective tissue and bones certainly become more fibrous with osteophytic formations developing by the 5th and 6th decades of life (12).
Anatomy
The formation of the sacroiliac joint (SIJ) consists of the articular surfaces of the sacrum and iliac bones (figure 2). The sacrum is a large triangular bone situated at the base of the vertebral column and comprises of five fused vertebrae wedged between the two iliac bones. Iliac nerves exit the foramen anteriorly and posteriorly. The sacral (anterior) aspect of the SIJ is lined with hyaline cartilage and the iliac side with fibrocartilage (7, 9).
The primary purpose of the SIJ is to maintain stability which is achieved by the union of the iliac ridge surface which 'sits' on the depressed sacral surface (6). The joint's movement is also minimised via the dense ligamentous network and surrounding muscle attachments which guide movement and enhance the stability to the pelvic bones (figures 4 and 5) (6).
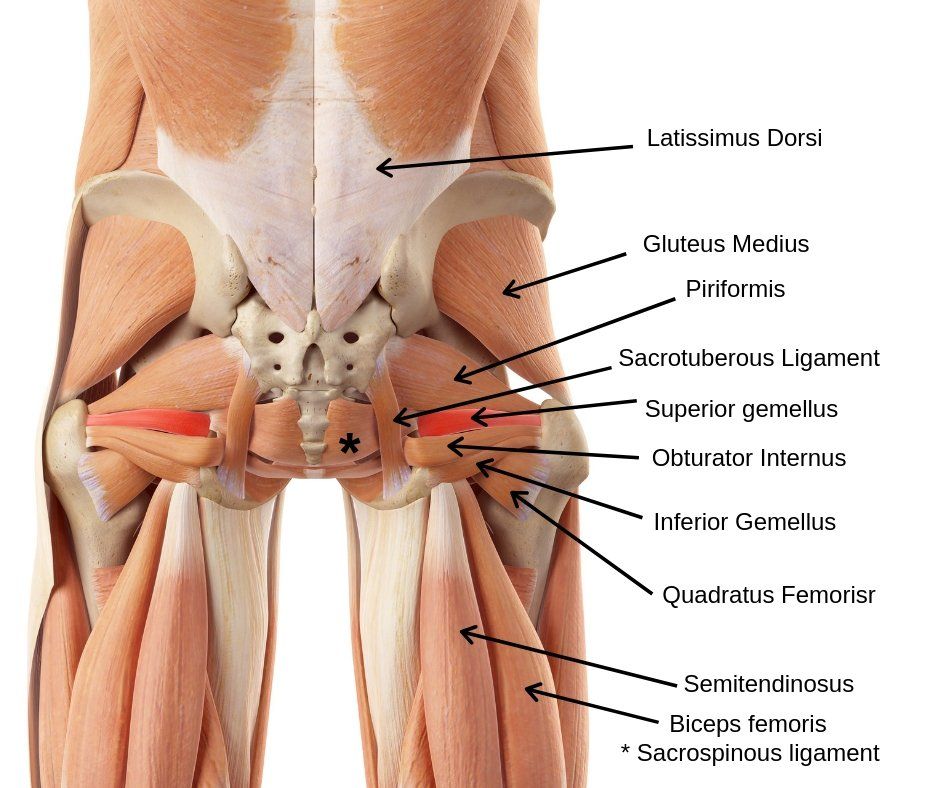
Muscles
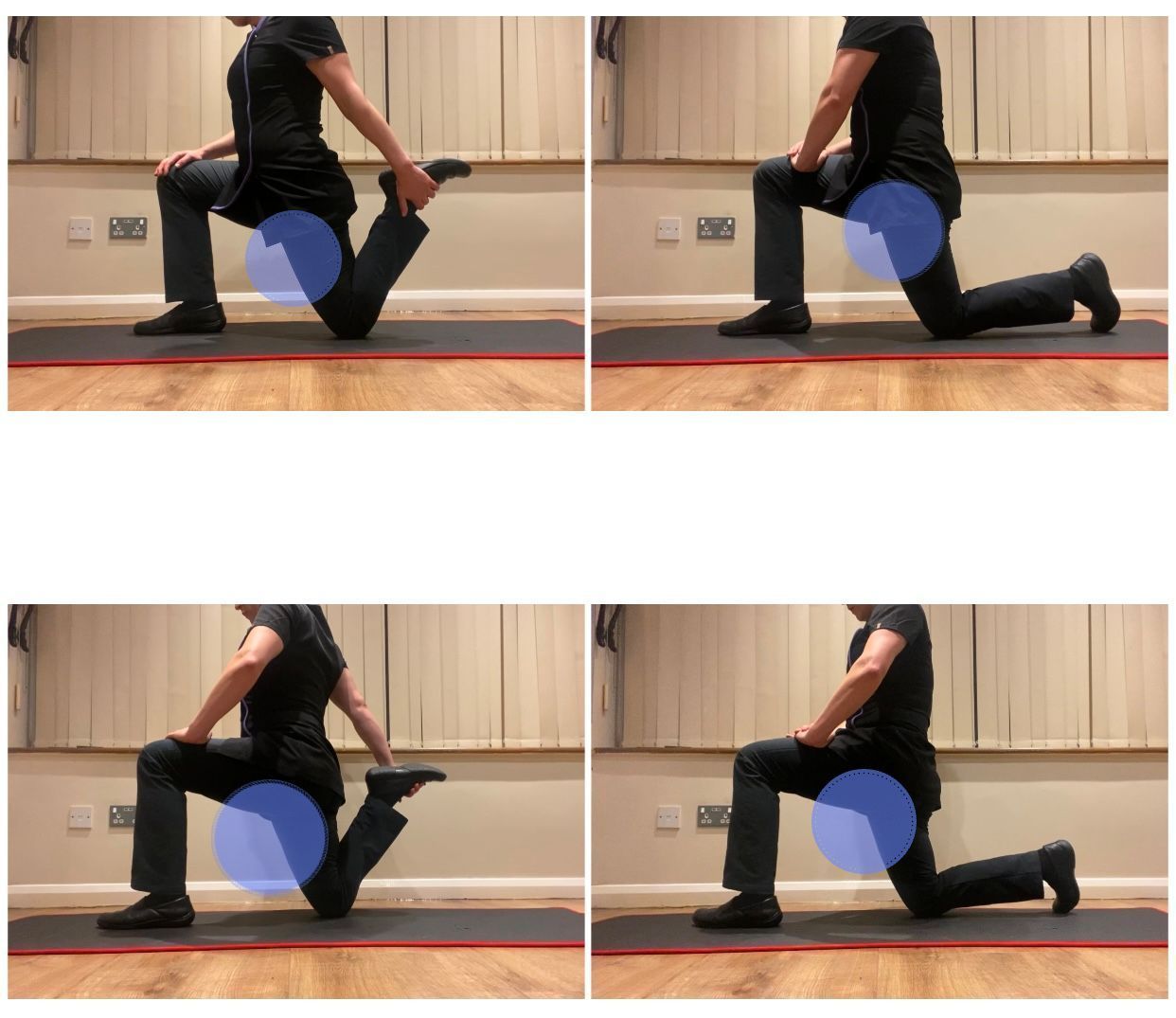
The SIJ is surrounded by the most largest and powerful muscle groups in the body and although none of the below muscles directly influences the movement of the joint, motion can still occur at the SI joint as a result of their contraction (figure 3). According to Schamberger (2012), there are 22 muscles that have an impact on the SI joint movement ranging from latissimus dorsi proximally and sartorius distally.
The primary muscles that connect to the SIJ ligaments include:
- Gluteus maximus
- Piriformis
- Biceps femoris
- Latissimus dorsi
From previous cadaver studies, gluteus maximus is of particular interest as it attaches to the sacrotuberous (ST) ligament (figure 5). They also discovered that the ST ligament can unilaterally or bilaterally be fused with the tendon of the long head of biceps femoris at its origin (12). The significance of the load application to the sacrotuberous ligament is important as studies have shown a significantly diminished ventral (forward) rotation at the base of the sacrum and increased compression of the sacrum against the iliac surfaces can further reduce movement of the SI joint and create too much ‘force closure’ (explained below) (12).
Other structures and muscles that support the joint are (7):
- Thoracodorsal fascia
- Gluteus minimus
- Quadratus lumborum
- Erector spinae
Anatomically and biomechanically, the sacroiliac joint shares the same muscles as the hip joint, further suggesting that both joints are directly related by force and weight-bearing and that the SIJ is unable to function in isolation (9).
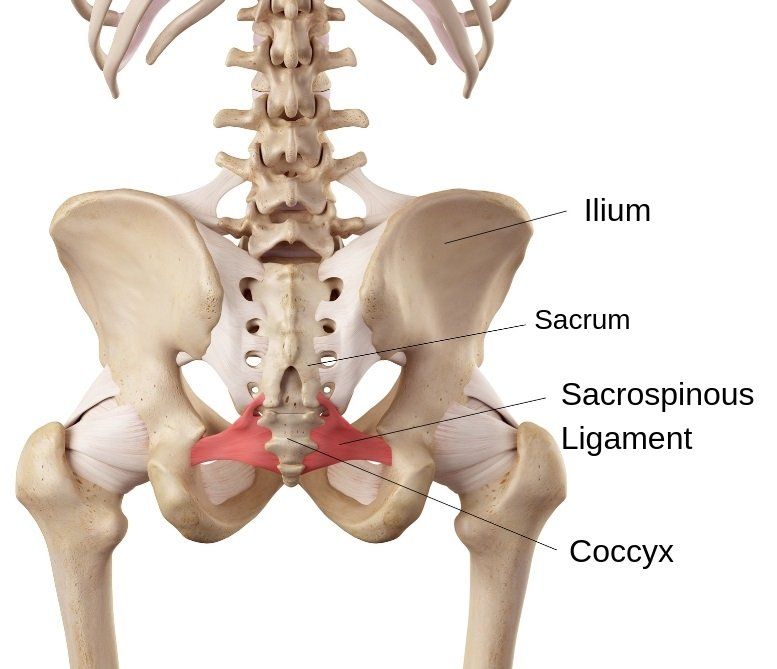
Ligaments
The role of the ligaments which attach to the sacroiliac joint is to limit range of motion, but hormonal influences can increase joint laxity in females, especially during pregnancy. Muscular attachments also contribute to stability of the sacroiliac joint.
The joint is surrounded by a capsule and ligaments which can be viewed from figures 4 and 5:
* The iliolumbar ligament
* Interosseous ligament.
* Sacrotuberous ligament - known for being the strongest ligament supporting the SIJ and in the body.
* Sacrospinous ligament.
Innervation
The
neural innervation of the posterior aspect of the SI joint is better understood
than the ventral (or anterior) region which is more relevant for treatment
purposes (2). Generally, the innervation of the posterior SI joint is mainly from
branches L4-S3 dorsal rami (2).
The
innervation of the ventral branches tend to stem from the ventral rami L5-S2
and possibly L4. Other literature supports the theory that the superior gluteal
and obturator nerves may also contribute which may explain how lower back pain can radiate into the buttocks or lower leg in
the involved side (2).
Neural innervations and the presence of nociceptors (which respond to harmful
stimuli) for pain are detected in both the joint capsule and posterior
ligamentous tissues of the sacroiliac joint (11).
Presentation and Pain Patterns of SIJ Dysfunction
Diagnosing and treating SIJ dysfunction can be challenging with its inconsistent presentation (6).
However, the most consistent factor for identifying SIJ pain is unilateral pain below L5 (6).
SIJ commonly presents with localised referred pain including(6):
· Lower buttock pain, which is as common as 94% of all cases (6).
· Lower lumbar region pain (72%).
· Lower extremity (50%)
· Leg pain
· Groin pain (14%)
· Hip pain
· Muscle spasms, with the most common muscle groups involving the hamstrings, hip flexors and quadriceps (6).
Symptoms can be described as dull and achy to sharp and stabbing sensations. Aggravating factors include all types of physical activity including bending climbing, lifting and rising (from the chair or car)(6).
SIJ and Function
- Transfers loads generated by gravity and the weight of the trunk and upper body to the ilia and onto the ischial tuberosities whilst sitting and through the hip joints to the lower extremities when standing (12).
- Transfer weight in opposite directions whilst standing, walking or falling.
- Shock Absorber particularly at heel strike during gait(12).
- Reduce translational forces or shearing between the iliac and sacral surfaces.
- Aid delivery during parturition.
SIJ and Movement
The of study SIJ movement has been heavily researched and there is much debate over whether movement can occur. Overall, motions of the SIJ are limited with rarely exceeding 3 degrees of movement (6).
The SIJ is six times more resistant to medial (middle) directed forces compared to the lumbar spine, but only has one twentieth of the resistance in axial compression and half of the resistance in rotation (6).
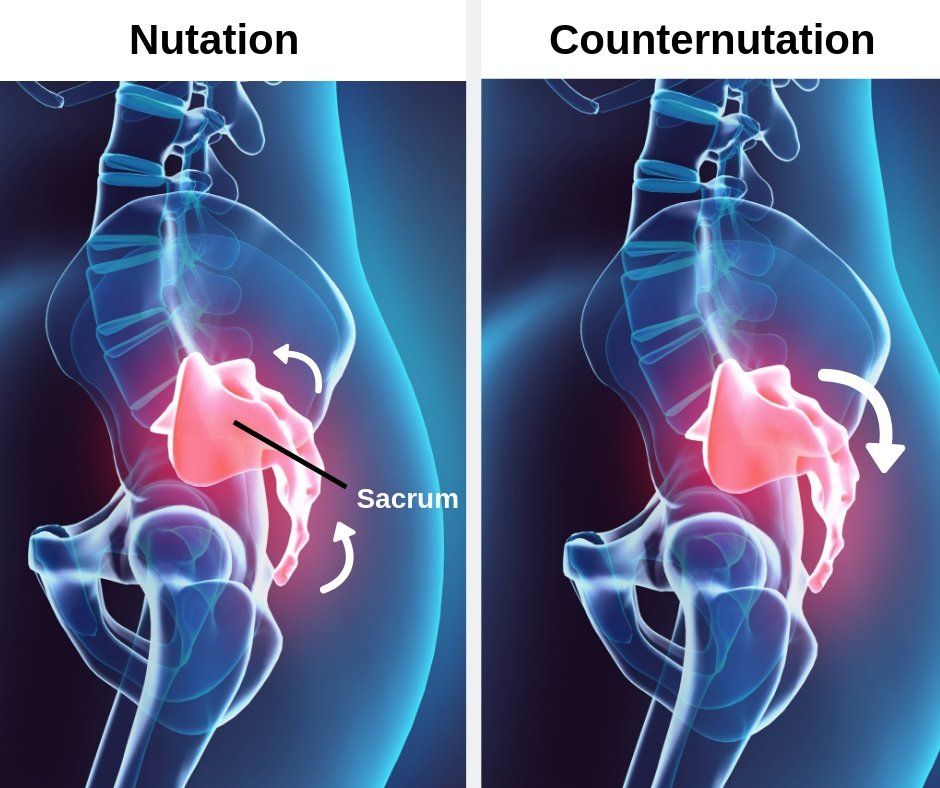
Form/ Force Closure, Sacral Counternutation and Nutation
Form Closure
Refers to the stability provided by the joint’s structure and supporting surrounding tissues such as the capsule and ligamentous structures and is derived by the following:
1.) The triangular shape of the sacrum which allows the bone to fit neatly between the innominates (or ilia) ‘like a keystone in a Roman arch’ (12).
2.) The sacrotuberous and sacrospinalis ligaments aid stability and minimise shearing.
3.) The increasing joint friction detected with advancing age as a result of: a.) the formation of the interlocking ridges and grooves. b.) roughening of the joint surfaces, which usually starts from the deterioration of the fibrocartilagenous covering of the iliac surface (12).
Force Closure
Refers to additional forces provided by muscles and myofacial structures that surround the SIJ joint which ensures stability during certain activities (12). SI joint force closure can be achieved by active forces (from e.g. muscles) which result in nutation of the sacrum or anterior rotation of the sacral base by contraction of surrounding muscles e.g. multifidi, extensor spinae or sacrospinalis muscles (figure 6) (12). Nutation creates a tightening of the interosseous, sacrotuberous and sacrospinous ligaments which facilitates the force closure mechanism and increases compression of the SI joint articular surfaces and aid stability of the joint for load transfer (12).
Force closure also arises from the contraction of the ‘inner’ and ‘outer’ myofascial units, or ‘core’ muscles which help to stabilise the pelvis, lumbar spine and hip joints or ‘lumbo-pelvic-hip complex' (12). Force closure of the SI joints will suffer as a result of problems such as (12):
1. Muscle weakness or atrophy.
2. Inadequate recruitment of muscles in one or several interacting muscle 'slings', which can also result in weakness.
3. Uncoordinated contraction and relaxation of muscle systems, resulting in failure to provide adequate stability and a consistent control of motion (12).
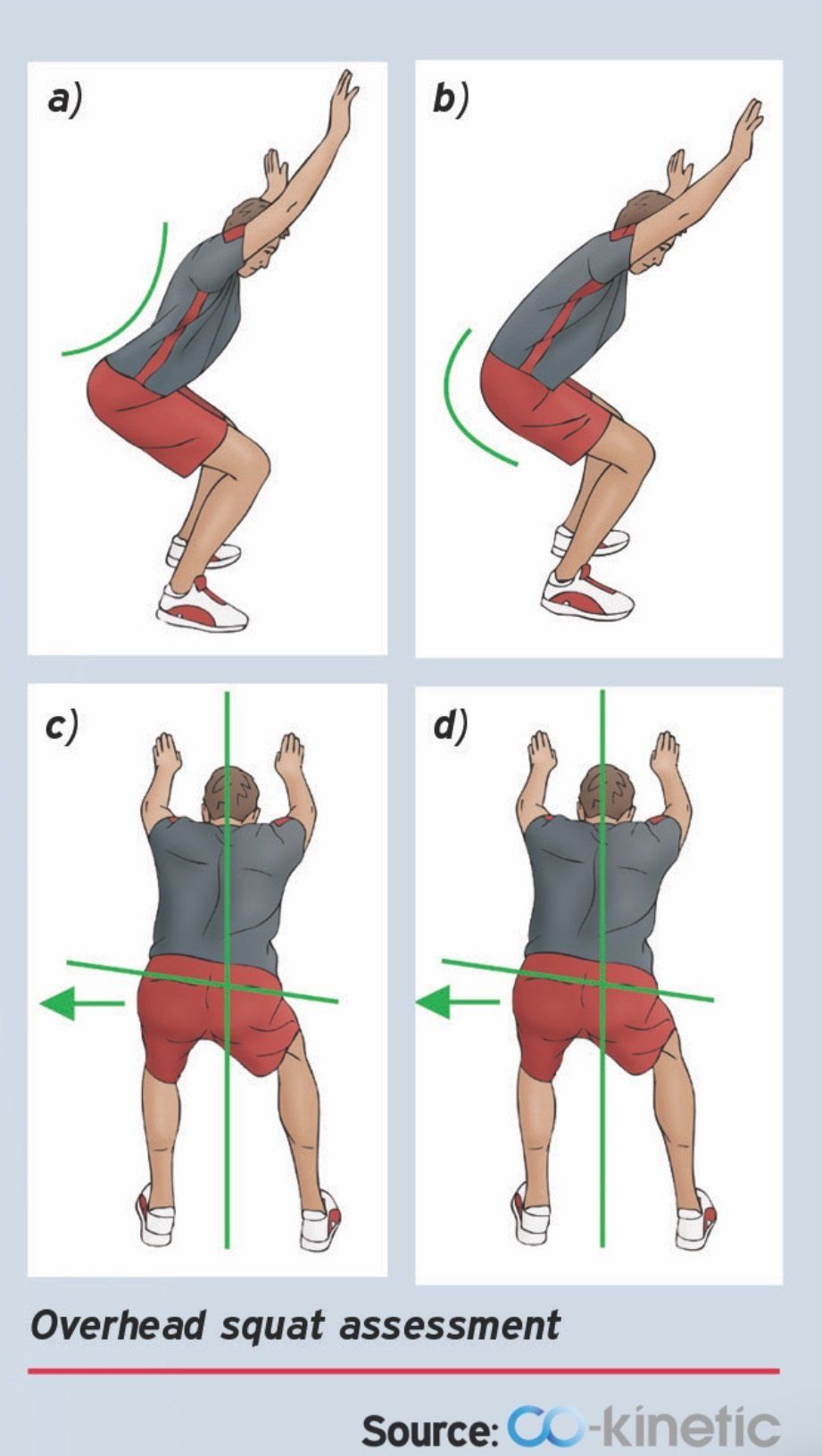
Movement patterns that a patient starts to use to compensate for insufficiencies from e.g. weakness, impaired muscle tension and control can result to abnormal stresses on the musculoskeletal systems and may lead to an eventual decompensation of the lower back, pelvis, hip and knee joints (12). An increased progression of degenerative changes, ligament laxity and joint instability could be the eventual end result of these compensations (12).
Cause of SIJ Pain
The body continues to compensate and make adaptations long after an initial injury which can lead to a gradual, slower increase in intensity of symptoms and is otherwise termed an "insidious onset" (1). The biomechanical adaptations can lead to muscle imbalances by becoming either overactive and hypertonic or underactive and hypotonic.
Trauma
Hansen and Helm(2003) consider the SIJ to be as a result of acute trauma from activities such as:
- Heavy or prolonged lifting and bending
- Torsional (rotational) strain.
- A fall onto the buttocks.
- A rear-end motor vehicle accident.
- Performing the golf swing.
- Throwing (baseball, throwing sports in athletics (discus, shot putt, javelin), American football).
- Figure skating.
- bowling.
- Constant sitting on the affected side.
- Constant lying on the affected side.
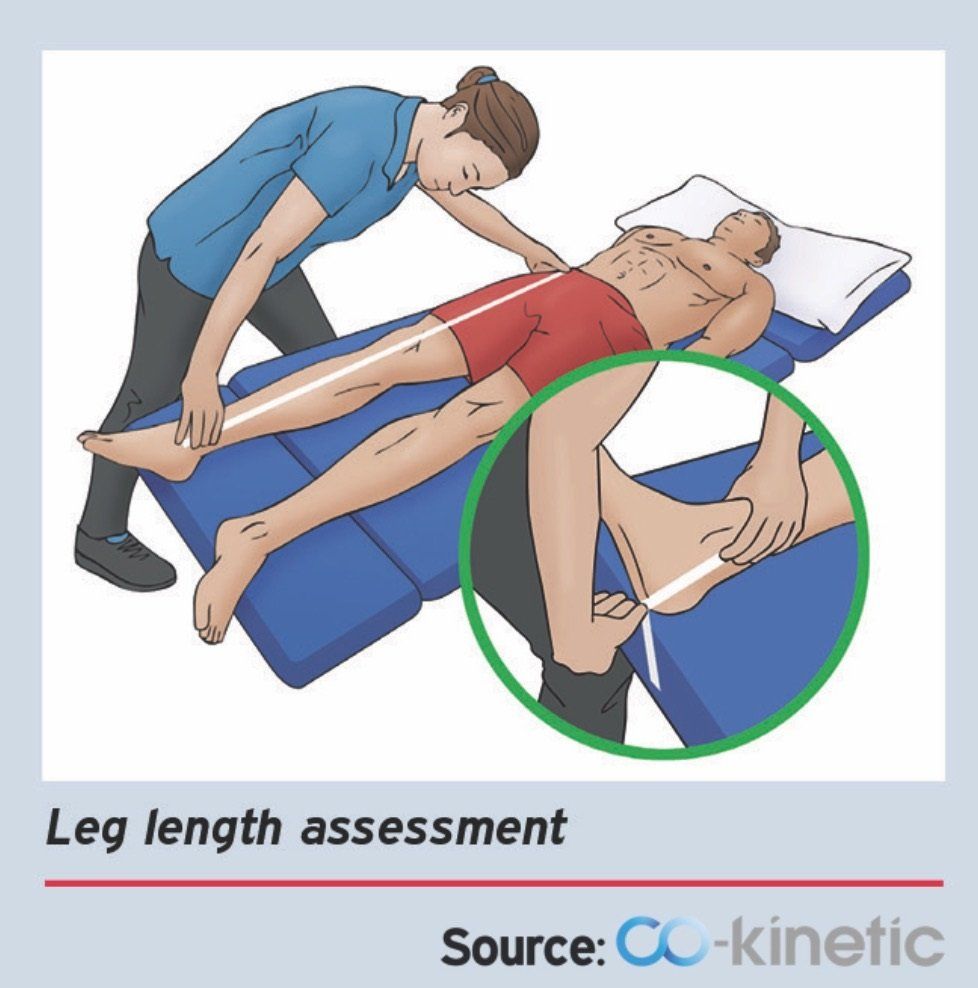
Cohen et al., (2013) describe how the main mechanism of injury to the SIJ can be best described as a combination of axial loading and rotation. Injury to any of the surrounding structures of the SIJ can be a source of pain. Other causes may include (2):
- Arthritis.
- Spondyloarthropathies (e.g. ankylosing spondylitis (AS), reactive arthritis, psoriatic arthritis, and enteropathic arthritis (EnA)).
- Ankylosing spondylitis (AS): an inflammatory rheumatic disease that involves the spine and SI joint and manifests as spondylitis and sacroiliitis (3).
- Leg length discrepancy.
- Lumbosacral transitional vertebrae (LSTV).
- Gait and biomechanical abnormalities.
- Persistent strain/ low grade trauma (e.g. jogging)
- Scoliosis.
- Pregnancy - one sided weight bearing, exaggerated lordotic posture, third-trimester hormone-induced ligamentous relaxation, pelvic trauma associated to parturition (2).
- Spinal surgery.
Pregnancy
Pregnancy can be a result of SIJ pain due to weight gain, exaggerated lordotic posture, third trimester hormone-induced ligamentous relaxation and the pelvic trauma associated with parturition. Ostgaard et al., (1991) found that SIJ pain comprised the majority of lower back pain cases throughout a nine month period (2). Gutke et al., (2006) discovered that common presentations of pain with SIJ dysfunction included pelvic girdle pain (PGP) and lumbar pain or a combination of both pelvic girdle and lumbar pain (2).
Spine Surgery
Spine surgery is a very common but underappreciated source of SIJ pain especially operations that involve fusion to the sacrum (2). A study by Ivanov et al. (2009) found increased SIJ stress post surgery was least after an L4 to L5 fusion but greatest if performed at L4 to S1. This is supported by Ha et al., (2008) who found that the incidence of SIJ degeneration is higher in patients with a fusion down to S1 than in patients with fusion down to L5 (16).
A history of iliac crest bone graft harvesting is another potential risk factor for SIJ pain and can result in disruption of the ligamentous and synovial portions of the SI joint (16). But, there are conflicting studies on this topic area (16).
Yoshihara (2012) note that there are three possible causes of SIJ pain post surgery:
(1) Increased mechanical load transfer onto the SIJ after fusion.
(2) Bone graft harvesting in the iliac crest close to the joint and
(3) A misdiagnosis of SIJ syndrome before fusion.
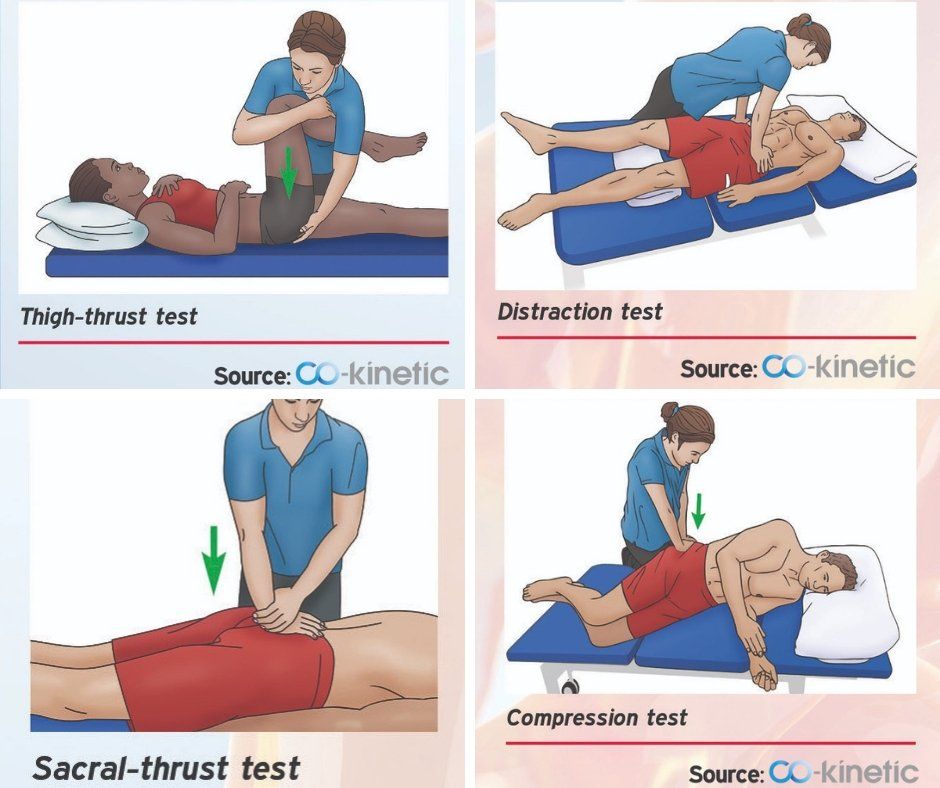
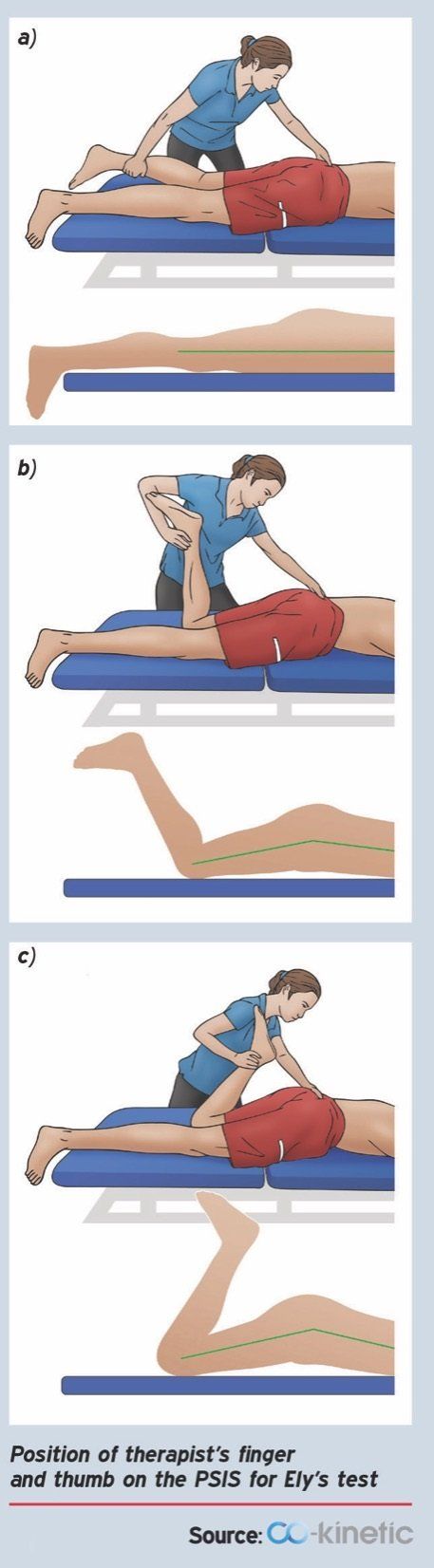
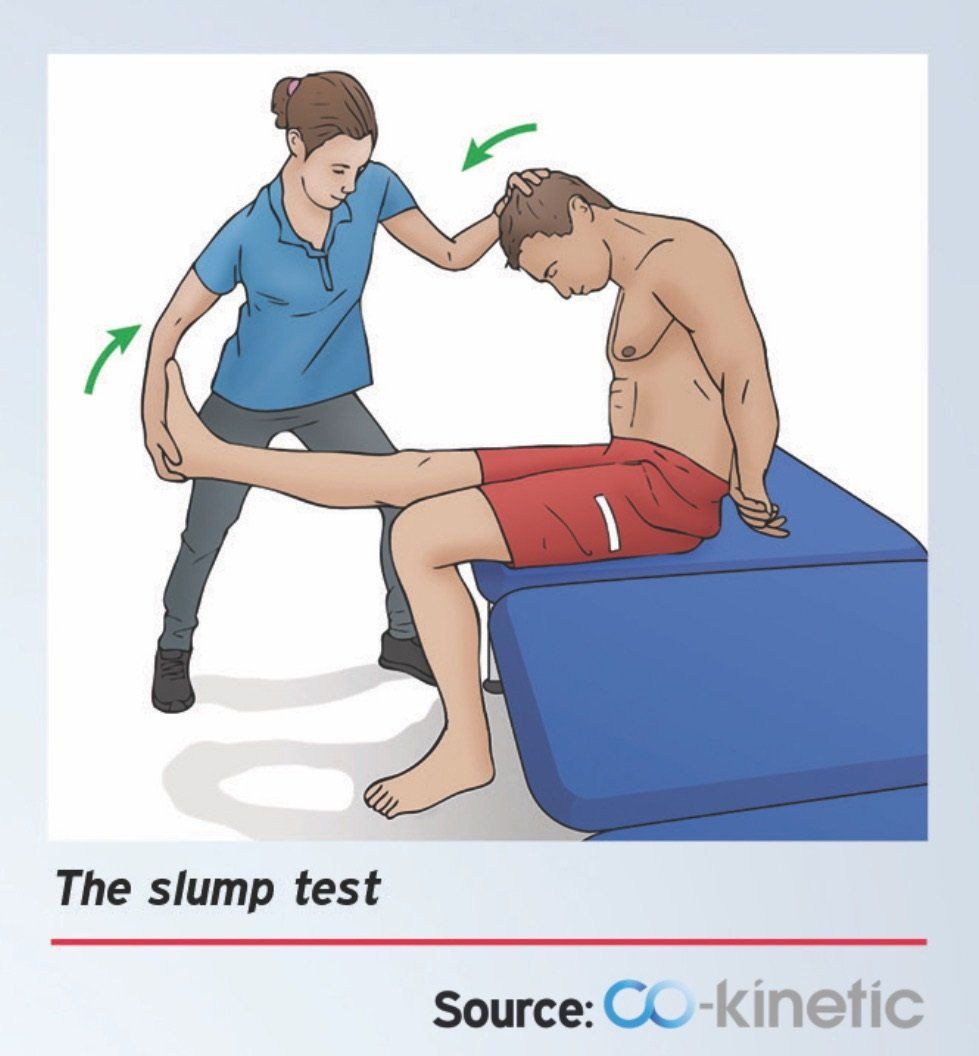
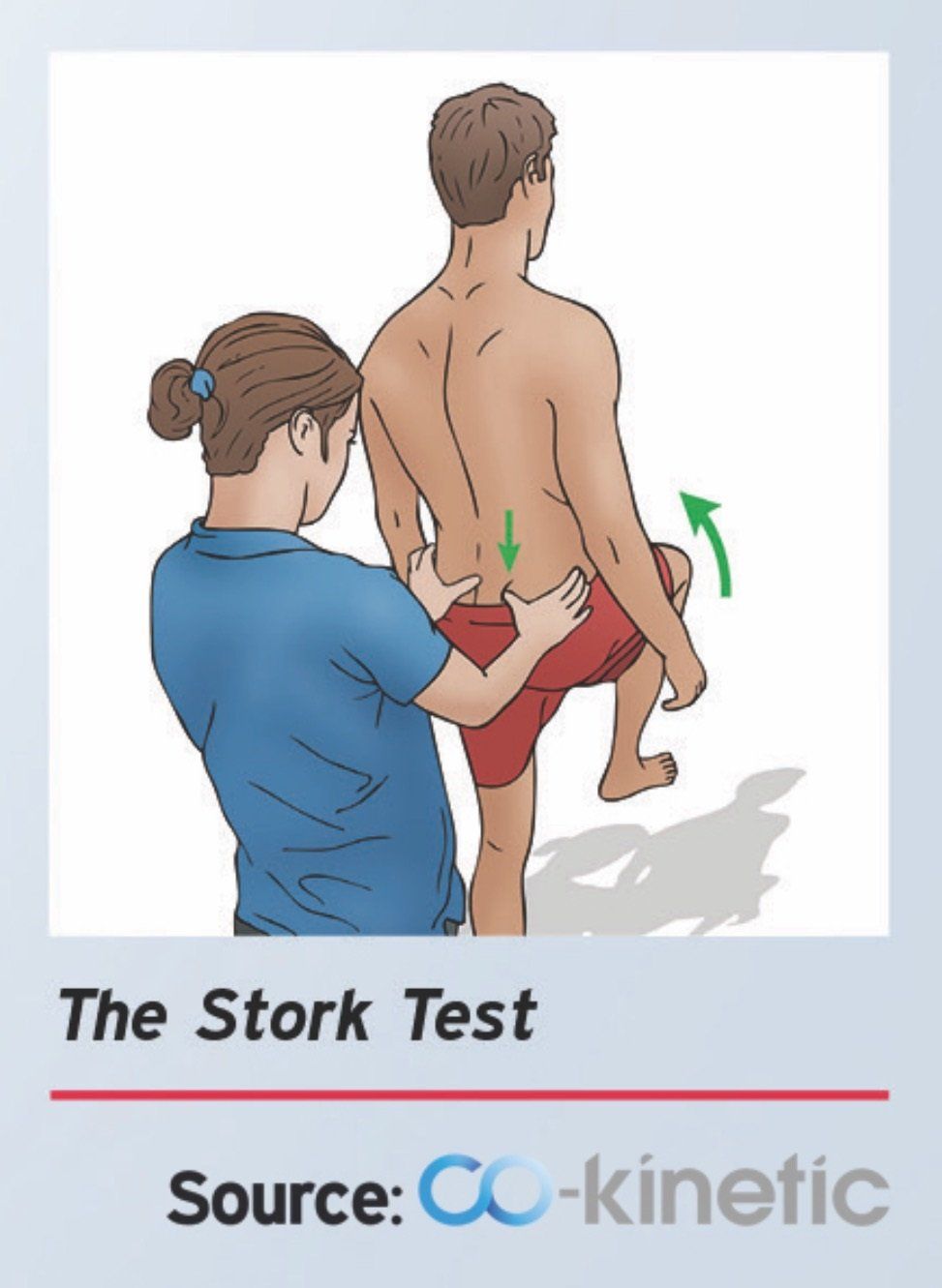
Assessment
However, previous studies have reported that there is not one single specific physical examination that can accurately identify a painful SIJ or define which structures are actually stressed (13).
Examples of these tests include:
1.) Patrick’s test
2.) Yeoman’s test
3.) Gaenslen’s test
4.) Gillet’s test
5.) Compression test
6.) Sacral sulcus tenderness,
7.) Sacral thrust test
8.) Thigh thrust test.
Most recent evidence shows that a minimum of three SIJ pain-provocation tests (out of four) must reproduce the patient's pain before the pain can be considered to be originating from the SIJ. These tests include the distraction, compression, thigh thrust and sacral thrut tests (figure 7) (13, 15).However, it must be noted that neither a client's case history nor positive SIJ provocation tests in isolation or in combination can confirm a clear diagnosis of SIJS (13).
References
1.) Clayton, P. (2016) Sacroiliac Joint Dysfunction and Piriformis Syndrome The Complete Guide for Physical Therapists, Lotus Publishing, Chichester England.
2.) Cohen, S. P., Chen, Y., Neufeld, N. J., (2013) Sacroiliac Joint Pain: A Comprehensive Review of Epidemiology, Diagnosis and Treatment, Expert Reviews Ltd, 13; 1: 99–116.
3.) Cohen, S., P. (2005) Sacroiliac Joint Pain: A Comprehensive Review of Anatomy, Diagnosis and Treatment, Anesth Analg, 101: 1440-53.
5.) Ha K, Lee J, Kim K (2008) Degeneration of sacroiliac joint
after instrumented lumbar or lumbosacral fusion. Spine 33:1192–1198.
6.) Hamidi-Ravari, B., Tafazoli, S., Chen, H., Perret. (2014) Diagnosis and Current Treatments for Sacroiliac Joint Dysfunction: A Review, Current Physical Medical Rehabilitation, Springer Science and Business Media New York; 2: 48-54.
7.) Hansen, H. C., Helm, S. (2003) Sacroiliac Joint Pain and Dysfunction, Pain Physician; 6: 179-189.
8.) Ivanov AA, Kiapour A, Ebraheim NA, Goel V. Lumbar fusion leads to increases in angular motion and stress across sacroiliac joint: a finite element study. Spine 34(5), 162–169 (2009).
9.) Kibsgard, T. J., Rohrl, S. M., Rosie, O., Sturesson, B., Stuge, B. (2017)
Movement of the sacroiliac joint during the Active Straight Leg Raise test in
patients with long-lasting severe sacroiliac joint pain, Clinical Biomechanics; 47: 40-45.
11.) Sahin, O., Harman, A., Akgun, R. C., Tuncay, I. C. (2012) An Intraarticular Sacroiliac Steroid Injection Under the Guidance of Computed Tomography for Relieving Sacroiliac Joint Pain: A Clinical Outcome Study with Two Years of Follow Up, Turk Rheumatol, 27; 3: 165-173.
12.) Schamberger, W. (2012) The Malignment Syndrome: Diagnosing and Treating A Common Cause of Acute and Chronic Pelvic, Leg and Back Pain, Churchill Livingstone Elsevier.
13.) Slipman, C. W., Sterenfeld, E. B., Chou, L. H., Herzog, R., Vrestilovic, E. (1998) The Predictive Value of Provocative Sacroiliac Joint Stress Maneuvers in the Diagnosis of Sacroiliac Joint Syndrome,
14.) Snijders, C. J., Hermans, P. F. G., Niesing, R., Spoor, C. W., Stoeckart, R. (2004) The Influence of Slouching and Lumbar Support on Iliolumbar Ligaments, Intervertebral Discs and Sacroiliac Joints, Clinical Biomechanics.
15.) Szadek, K. M., van der Wurff, P., van Tulder. M. W., Zuurmond, W. W., Perez. R. S. (2009) Diagnostic Validity of Criteria for Sacroiliac Joint Pain: a Systematic Review, The Journal of Pain, 10; 4: 354-368.
16.) Yoshihara, H. (2012) Sacroiliac Joint Pain After lumbar/ lumbosacral Fusion: Current Knowledge, Eur Spine J, Springer-Verlag, 21: 1788-1796.